Urinary System Physiology: Glomerular Filtration and Autoregulation
Document from Prof. Pellicciari about Urinary System. The Pdf explores the physiology of the urinary system, detailing renal filtration, reabsorption, and secretion processes, and the mechanisms of glomerular filtration rate (GFR) autoregulation, useful for University Biology students.
See more37 Pages

Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Introduction to the Urinary System
If we want to define the urinary system, we refer to the different organs that work to remove wastes from the blood and eliminate them through urine. This system involves kidneys but also associated structures and it works to remove excess water, salt, acid, and other electrolytes from the plasma and eliminates - them in the urine - to regulate the chemical composition, volume and electrolyte balance in the blood - to help maintain the acid-base balance of the body. It is important to maintain a balance of electrolytes because all the functions of the cell depend on the maintenance of a stable concentration of salt, acid and other electrolytes in the internal fluid environment. Cell survival also depends on continuous removal of toxic metabolic wastes and the urinary system works to allow this, to maintain the homeostasis by managing the volume and the composition of fluid reservoirs, primarily blood. This specific role is covered by the kidneys. The kidneys play a specific role in the maintenance of homeostasis by regulating the concentration of many plasma constituents and by eliminating all metabolic wastes. The special relevance is the ability of the kidneys to regulate the volume and solute concentration, (osmolarity) of the internal fluid environment by controlling salt and water balance.
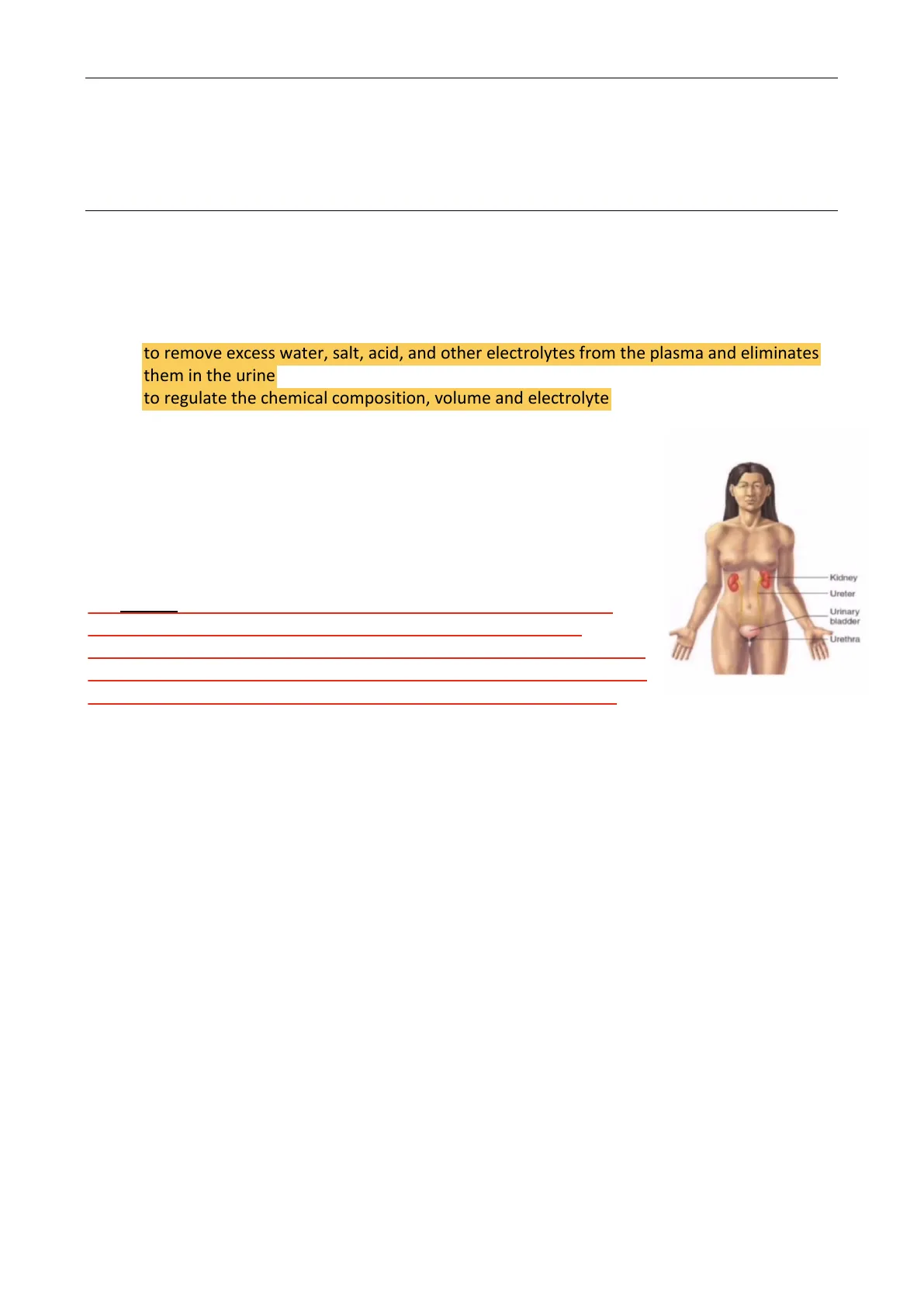
Kidney Ureter Urinary bladder Urethra
The urinary system is composed of several organs that include: - kidneys - ureters - urinary bladder - urethra The final function of these organs is to filter the blood and to eliminate the excess of ions and metabolic wastes with water that will leave the body in the form of urine.
Functions of the Urinary System
It works to filter the waste product from the blood and when we talk about "waste products" we refer to water and sodium chloride (NaCl) and this operation is regulated in conjunction with other systems as the cardiovascular, the endocrine and the CNS.
Waste Products Eliminated by the Urinary System
Waste products are: . ammonia and urea that are formed when amino acids are broken down; · uric acid formed when nucleic acids are broken down; . the creatinin that derives from the muscle; . and all of the end products of haemoglobin metabolism; · hormone metabolites;
1Physiology II. #33.2 - Prof. Pellicciari - Urinary system Page 2 of 5
- foreign substances (drugs and food ingested);
Filtration, reabsorption and secretion are the processes through which the kidneys filter the blood and finally, we have the formation of the urine. Filtration is not the only function of the urinary system but it also works to:
- conserve valuable nutrients. For example, it ensures glucose, amino acids and other valuable nutrients are not lost from the urine;
- regulate ions level in the plasma: it regulates the level of electrolytes in the plasma by regulating the amount of sodium, potassium, chloride and other ions lost in the urine;
- regulate blood pH by regulating the amount of bicarbonate and hydrogen ions lost in the urine;
- regulate blood volume by releasing a hormone called renin that after a series of reactions controls salts and water loss at the kidneys and also by adjusting the volume of water lost in the urine;
- regulation of RBCs production by releasing erythropoietin when we have a detection of low levels of oxygen. Having more RBCs allows the blood to transport more oxygen
- store urine in the bladder;
- excrete urine through the urethra from the urinary bladder to outside of the body;
- produce and secrete renin, erythropoietin and also vasoactive substances that lead to the modulation of renal blood flow and along with angiotensin II affect the systemic blood flow.
If we want to describe the urinary system from an anatomical point of view it consists of the urine forming organs that are the kidneys and other structures that only carry the urine from the kidney to the outside. All the urinary processes related to the filtration, absorption and secretion occur ONLY in the kidney.
Kidney Functions
In the kidneys, we can define several parts: cortex, medulla, renal pelvis and nephrons - They filter waste products from the bloodstream and convert this fluid that is called filtrate into urine that passes through the urinary tract which contains all of the other organs of the urinary system and allows transport outside this filtrate. - the kidneys are primarily responsible for maintaining stable volume, electrolyte composition and osmolarity of the extracellular fluid, so the function of the kidney is to adjust for variation in ingestion of water, salt, and other electrolytes. - When you have heavy sweating, vomiting, diarrhoea, or haemorrhages there is a loss of fluid and the kidneys work to adjust the urinary output of ECF constituents to compensate for abnormal losses. - It eliminates toxic metabolic wastes and foreign compounds from the body. We are not able to eliminate them as solids from the body but they must be excreted in a specific solution, in this way the kidneys are obligated to produce a minimum volume of around 500mL of waste-filled urine per day, it is functional for the normal working of our body. The origin of the water that is eliminated in the urine is the plasma. If we don't have water the plasma volume falls to a
CREATININE, AMMONIA AND URIC ACID: 0.2% DISSOLVED SALTS AND OTHER IONS: 2.8% WATER: 95% UREA: 2%
2Physiology II. #33.2 - Prof. Pellicciari - Urinary system Page 3 of 5 fatal level because the available water is removed to accompanied the removal of wastes.
Anatomy of the Urinary System
General Anatomy of the Kidney
To better understand the function of the kidney we have to start from the anatomy. Each kidney, that is this bean-shaped organ is supplied by a renal artery and a renal vein, the first one enters the kidney and the second one leaves it. The kidney acts on the plasma to produce urine, conserving materials to be retained in the body and eliminating materials into the urine. After the urine is formed it is drained into a central collecting cavity, the renal pelvis, located at the medial inner core of each kidney. From the renal pelvis, urine is transported into the ureter, a duct that exits at the medial border close to the renal artery and vein. There are two ureters empty into the urinary bladder that temporarily stores the urine. This latter is a hollow, muscular organ that can be related to the capacity to store the urine until the final urination.
Kidney Ureter- Bladder- Sphincter Urethra Uterus urethra
Clinical Note: Benign Prostate Hyperplasia
It is a common condition in old men in which we have an enlargement in a noncancerous way of the prostate, this creates a pressure of the urethra and this can lead to several symptoms related to the function of the urinary system as a frequent need to urinate, the feeling of incomplete bladder emptying and other symptoms related to urination.
NORMAL Bladder neck Pros itic- Prostate culatory duct ENLARGED Bladder neck Prost uret rostate
Kidney Anatomy
The kidney is composed by: - the outer region that is called the cortex - an inner region that is called the medulla - and the renal columns. These renal columns consist of connective tissue extensions that radiate downward from the cortex through the medulla and their role is to separate the
3 Finally, there is the urethra. There are in anatomical terms differences between males and females in whom it is respectively 20 cm and 3-4 cm long. Specifically, when we talk about the male urethra it starts from the prostate gland which is located below the bladder in front of the rectum and its main job is making fluid for semen. During the ejaculation, sperm makes the testicles move to the urethra, at the same time fluid from the prostate and the seminal vesicles also move there and this mixture of semen goes through the urethra and the penis.
Umbilicus 8 Superior wall Labia majora Mons pubis of distended bladder Prepuce of clitoris Clitoris (head) Labia minora Urethral Superior wall- Fourchette Vestibule ..... of empty bladder orifice Vaginal Pubic symphysis orifice Hymen (ruptured) Anu Urethra Opening of the duct -
Physiology II. #33.2 - Prof. Pellicciari - Urinary system Page 4 of 5 most characteristic features of the medulla: the renal pyramids and renal papillae. The role of the renal columns is also to divide the kidney into different lobes and so to create a supporting framework for vessels that enter and exit the cortex. Both the pyramids and the cortex around the renal columns form the kidney's lobes. About the renal papillae, they represent a bundle of the connective duct and the work to transport the urine made from the nephron to the calyces of the kidney for excretion. An important part of the kidney is the renal ileum that represents the point in which we can observe several structures that enter into the kidney and exit from the kidneys that are vessels, nerves, lymphatics and ureters. Near to the ileum, we can see the presence of the renal pelvis, which is formed by two calyces that are the major and the minor calyx in the kidney. An important role in terms of structure that serves the kidney and that enters and exits from this point is the renal artery and the renal vein. The renal artery is formed directly from the descending aorta and the renal vein returns the cleansed blood to the inferior vena cava.
Cortical blood vessels Intertobar blood vessels Renal vein- Renal Pyramid hilum Renal- nerve Renal artery Papilla Medulla- Ureter Cortex Capsule Arcuate blood vessels Minor calyx Major calyx Renal pelvis Renal column
Microscopy of the Kidneys
We can consider the kidneys as a collection of several uriniferous tubules. These tubules consist of an excretory part that is called nephron and of a collectin duct also called collectin tubule. (Uriniferous tubules = nephron + collectin tubule)
Renal capsule Nephron Renal cortex Collecting duct Renal medulla - Minor calyx Renal papilla
When we talk about kidney we can say that they consist of numerous uriniferous tubules that are composed of Nephron and Collecting duct and they are accompanied by a capillary network that is called the vasa recta that runs parallel with the tubules and represent the countercurrent exchange system (that we will see in the next lesson) that can regulate the concentration of the urine. When we talk about absorption and secretion we refer to different processes that happen between the peritubular and tubular lumen.
The Functional Unit of the Kidney: Nephron
The functional unit of the kidney is the nephron. We can detect two different types of the nephron and now we see what they consist of, but if we want to describe the main component it consists of a renal corpuscle that is related to performing a specific function related to the filtration and it is composed by the glomerulus and the Bowman's capsule that surrounds the glomerulus. Other components are the renal tubules that are involved in reabsorption and secretion. The renal tubules are composed of: - the proximal convoluted tubule, - the tube of Henle, - and the distal convoluted lobule. The distal convoluted tubule of several nephrons empties into a single collecting duct or tubule.
4