Clinical Skills: Neurological Examination of Cranial Nerves
Document from Clinical Skills about Neurological Examination of Cranial Nerves. The Pdf provides a practical guide to the neurological examination of cranial nerves (I-XII), with detailed instructions for evaluating each nerve. It is useful for university students and healthcare professionals.
See more9 Pages

Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Clinical Skills: Neurological Examination
Cranial Nerves Overview
Notes:
- Sanitize your hands before touching your patient
- Tell the patient that during the exam you will have to get close and touch them
If they feel any discomfort, they should say it - Always tell the patient what you are about to do and ask for consent (I will do this, is
that ok?)
Demonstrate assessment of cranial nerves I - XII.
Before each nerve/nerves assessment discuss components and territory of
innervation.
Cranial Nerve I Assessment
Evaluate the patency of the nasal passages bilaterally by asking the patient to breath in
through their nose while the you occludes one nostril at a time.
Once patency is established, ask the patient to close their eyes.
Occlude one nostril, and place a small bar of soap or a small tube containing something with a
distinct odor near the patent nostril and ask the patient to smell the object and report what it
is.
Making certain the patient's eyes remain closed. Switch nostrils and repeat. Furthermore, ask
the patient to compare the strength of the smell in each nostril.
Very little localizing information can be obtained from testing the sense of smell. This part of
the exam is often omitted, unless their is a reported history suggesting head trauma or toxic
inhalation.
Cranial Nerve II Assessment
In a typical neurological examination, you would evaluate visual acuity (with a chart) and the
visual field.
Evaluation of the visual field:
- Sit in front of your patient eye
to eye. - Ask the patient to look at your
eyes. - Put your hands out on both
sides, midway between you
and your patients, around 50
cm apart, approximately 30 cm
above eye level.
· Wiggle your fingers (2nd or 2nd and 3rd) first on one side, than on the other, and
then together. Ask the patient to tell you on which side you are moving your fingers
.
Repeat with your hands approximately 30 cm below eye level.
Now, ask the patient to cover their right eye with their right hand and look at you in the
eyes. Instruct the patient to remain looking you in the eyes and say "now" when your fingers
enter from out of sight, into their peripheral vision. Once this is understood, cover your left
eye with your left hand (the opposite eye of the patient) and extend your right arm and first
2 fingers out to the side as far as possible. Beginning with your hand and arm fully extended,
slowly bring your outstretched hand, wiggling your fingers, towards the midline and notice
when your fingers enter your field of vision. The patient should say now at the same time
you see your own fingers. Do the same coming from the upper quadrant and lower
quadrants of the visual field. Now, use your right hand to keep on covering the left eye,
extend your left hand and do the same coming from the left. Repeat the same maneuver
with the other eye.
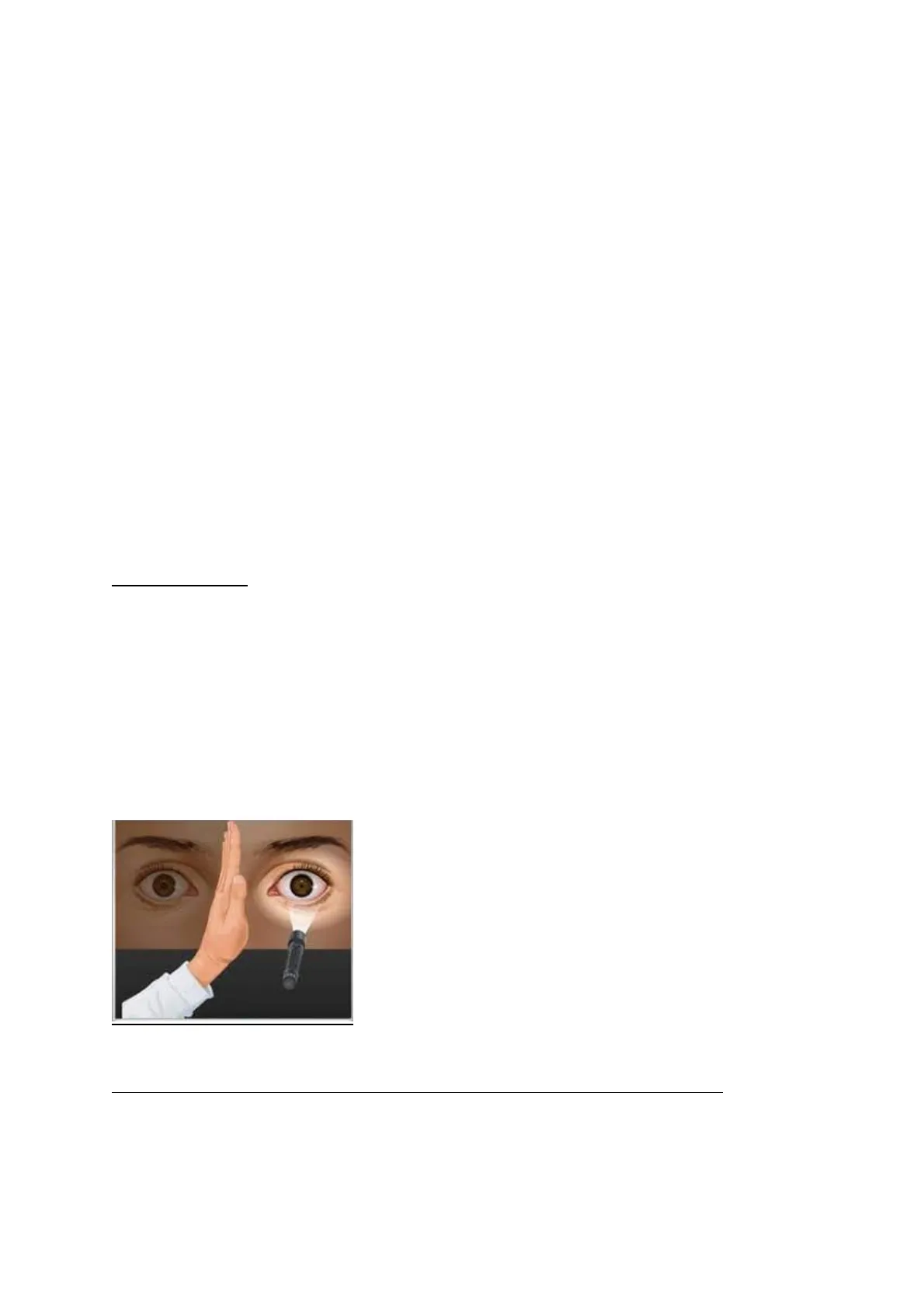
Cranial Nerves II and III Assessment
Response to light:
- Observe the pupils of the patient for size and symmetry
- Dim lights.
- Ask the patient to focus on an object in the distance (e.g. opposite wall).
- Observe the diameter of the pupils. Note the symmetry between the pupils.
- Next, hold one of your hands in the sagittal plane in front of the nose your patient.
Shine the penlight light obliquely into each pupil at a time and check both the direct
(same eye) and consensual (opposite eye) light responses in each pupil. Note the
rate of these reflexes.
Near response (checks pupillary constriction, convergence and accommodation):
- Test for pupillary constriction via accommodation by asking the patient to focus on
the tip of your finger or of a pencil/stick while you move it closer and closer to their
nose. - Hold finger at 10 cm from patient's nose
o Ask the patient to alternate looking into distance and at finger
o
Observe pupillary response
Normally, as the eyes accommodate to the near object the pupils will constrict. The test for
accomodation should also be completed in a dimly lit room. End the evaluation of cranial
nerves II and III by observing the pupils in a well lit room and note their size and possible
asymmetry.
Nerves of Oculomotion: III, IV, VI
- Position yourself in front of the patient and ask them to look at the tip of a stick, a
pen or of your finger. - Observe if the eyes are aligned, if there is drooping of the eyelids, if there is
nistagmus - Ask now the patient to follow the movement of a stick/pencil or finger in different
direction (without moving their head) and to tell you if and where they see it double.
In the meanwhile, observe if there is any sign of nystagmus. - One technique: Move the stick (keeping it vertical) first horizontally to the left and
then to the right. Get back in the central position, keep the stick horizontal and move
it upwards and then downwards. Before moving it downwards, ask the patient if you
can keep their eyes open by gently putting your fingers on the upper eyelids and
keeping them up while the patient is following the movement of the stick.
Do the same in the oblique directions: down to the corner on the left, then on the
right; up to the corner on the left and then on the right.
Another technique: Making a wide H in the air, lead the patient's gaze (1) to the
patient's extreme right, (2) to the right and upward, and (3) down to the right; then
(4) without pausing in the middle, to the extreme left, (5) to the left and upward, and
(6) down on the left.
Testing for the presence of saccades on the horizontal plane: position your stick to
the left of the patient and your finger to the right. Ask the patient to look,
alternating, to the right and to the left (say: "to the right, to the left", quite rapidly)
With this test you are looking for an internuclear ophthalmoplegia due to a lesion of
the MLB. It the patient has an internuclear ophthalmoplegia of the left MLB, when
the patient is asked to look to the right, the medial rectus of the left would not work
properly and the patient would show nystagmus during the abduction of the right
eye.
Cranial Nerve V Assessment (Motor, Sensory, Reflexes)
Motor Function of Cranial Nerve V
- First, palpate the temporal and masseter muscles while you instruct the patient
to bite down hard (clench their teeth). Note the strength of muscle contraction.
PALPATING TEMPORAL MUSCLES
PALPATING MASSETER MUSCLES - Next, ask the patient to open their mouth and then to open it against resistance
(you gently press the chin from below while the patient is trying to keep it open)
Ask the patient to move the lower jaw to the left and to right against the
resistance applied by your hand (to the right and to the left of the chin)
(pterygoid muscles).
Sensory Function of Cranial Nerve V
Start with soft touch using a wisp of cotton.
- First of all touch the skin at the top of the sternum and say to the patient "this is
soft touch) - Ask the patient to close their eyes and touch gently the skin of the forehead (V1)
first on one side and then on the other side. Ask the patient if they feel the touch
and if it is the same on both sides. Then test V2 (chick), and V3 (mandible)
Proceed in the same way for pain using with the pin-prick test. Ask the patient if
the sensation is of something sharp or dull
1
C2
=
III
C3
=
Reflexes of Cranial Nerve V
Corneal reflex
Ask the patient to look up and to the left as much as possible. Prepare a clean
wisp of cotton with a fine tip. Come from the side, avoiding the eyelashes, and
touch gently the cornea. Both eyes should blink as a reflex.
CN5 Reflex Testing
Jaw jerk reflex
Ask the patient to open the mouth fully and then to close it a bit, keeping it
relaxed. Put your index finger horizontally on the chin and then tap on it with the
hammer (normally absent or small. Brisk in UML).
Cranial Nerve VII Assessment (Motor, Sensory, Reflexes)
- Initially, inspect the face during conversation and rest noting any facial
asymmetry including drooping, sagging or smoothing of normal facial creases.
Motor Function of Cranial Nerve VII (Muscles of Facial Expression)
- Next, ask the patient the following:
Raise your eyebrows, as high as you can, as if surprised
Frow down, as angry as possible.
Squeeze your eyes really tight, as if you had soap in them. Now, I will
touch your eyes, trying to open them, don't let me
Show me your teeth
Blow out your cheeks and then keep blowing them out while I'm
trying to push them in with my fingers
Sensory Function of Cranial Nerve VII (Taste, Anterior 2/3 of the Tongue)
- Ask the patient: Have you noticed any change in your sense of taste?
- Now use salt and sugar: ask the patient to close their eyes and to stick out their
tongue. Sprinkle sugar or salt on the tongue - Ask the patient if sounds have become louder than usual
Reflexes of Cranial Nerve VII
- Corneal reflex
Cranial Nerve VIII Assessment
Auditory Function of Cranial Nerve VIII
- Ask the patient if they have any hearing problems. Ask the patient if they have
any hearing aid. - Position yourself to the left of the patient and use your right hand to press on
the tragus of the right ear (your right forearm is behind the head of the
patient); Whisper some numbers close to the left ear (first at around 15 cm of
distance and then at around 60 cm of distance, forearm length distance) and
ask the patient to repeat them. Do the same on the other side.
Vigorously rub your fingers together very near to, yet not touching, each ear and
wait for the patient to respond.
Vestibular Function of Cranial Nerve VIII
- Ask the patient to close the eyes and march on the spot. Usually, the patient
turns towards the side of the lesion
Cranial Nerves IX and X Assessment
- Ask the patient to swallow and note any difficulty doing so. Ask the patient if
they have difficulty in swallowing. - Note the quality and sound of the patient's voice. Is it hoarse or nasal?
- Ask the patient to open their mouth a wide as they can and tilt their head a
fraction backward.
Shine your penlight on the palate to see the palatal movements. - Ask the patient to say "AHH" and and observe the soft palate, uvula and
pharynx. Check the upper movements: the soft palate should rise
symmetrically; the uvula should remain midline and the pharynx should
constrict medially like a curtain. Often the palate is not visualized well during
this manuever. One may also try telling the patient to yawn, which often
provides a greater view of the elevated palate. - Ask the patient to cough
- Reflex: gag reflex
Cranial Nerve XI Assessment
- Look at the sternocleidomastoideod trapezius checking for wasting or
fasciculations - Ask the patient to shrug up their shoulder and check for possible
asymmetry. Then test the power of the muscle by asking the patient to do
the same against the resistance of your hands while they are pressing down. - To the test the left sternocleidomastoideok the patient to turn their head
to the right. Then, ask the patient to do it against the resistance of your
hand. Repeat this maneuver on the other side The patient should normally
overcome the resistance applied by the examiner.