Interpretation of Clinical Laboratory Tests from Wolters Kluwer Health
Document from Wolters Kluwer Health | Lippincott Williams & Wilkins about Interpretation of Clinical Laboratory Tests. The Pdf explains the origin of enzymes in the blood, their presence in health and disease, and the diagnostic importance of isoenzymes. This Science document for University students details lactate dehydrogenase (LDH) and creatine kinase (CK) in diagnosing myocardial infarction.
See more15 Pages

Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Interpretation of Clinical Laboratory Tests
BIOCD 1556 Lecture 4 Dr. Susan Viselli Interpretation of Clinical Laboratory Tests Introduction Laboratory tests often evaluate levels of enzymes in patients' blood samples. Most enzymes are normally found inside cells; many are located within cellular organelles. While a few enzymes are actively secreted into the plasma (fluid fraction of blood), most enzymes in healthy individuals are intracellular and have no physiological function in the plasma. The presence of elevated enzyme activity in plasma may indicate that enzymes have been released from damaged cells. Measurements of enzymes are routinely done for diagnostic purposes in diseases of the heart, liver, skeletal muscle, and certain other tissues/organ. The concentration of a particular enzyme in the plasma frequently correlates with the extent of tissue damage and may be useful in evaluating the prognosis for the patient.
TERMINAL OBJECTIVE: To understand the principles and practices for the use of enzymes in clinical diagnosis and to understand the organization of and interpretation of results in the serum chemistry profile.
Enabling Objectives for Clinical Diagnosis
Pathology Diagnosis
- Explain why enzymes in blood are useful in the diagnosis of pathology.
- List commonly measured enzymes and describe the tissue/organ source for each.
- Explain the patterns of LFTs predicted in various forms of liver injury.
- Describe interindividual and intraindividual variation and explain why critical differences calculations may be important.
- Describe the diagnostic usefulness of isoenzymes and explain how clinically important enzymes are measured.
Recommended Reading: LIR Biochemistry, 9th edition, pages 73-77
Origin of Plasma Enzymes
Most diagnostically important enzymes have intracellular functions and are normally present inside cells, either within an organelle or in the cytosol. Some other enzymes function in extracellular fluids other than blood plasma.
Enzymes are needed inside cells to catalyze reactions in biochemical pathways. When membranes (plasma and organelle) are damaged, the enzymes normally contained within their boundaries are released into fluids outside cells. Oftentimes the enzymes may be measured in samples prepared from whole blood drawn from a patient.
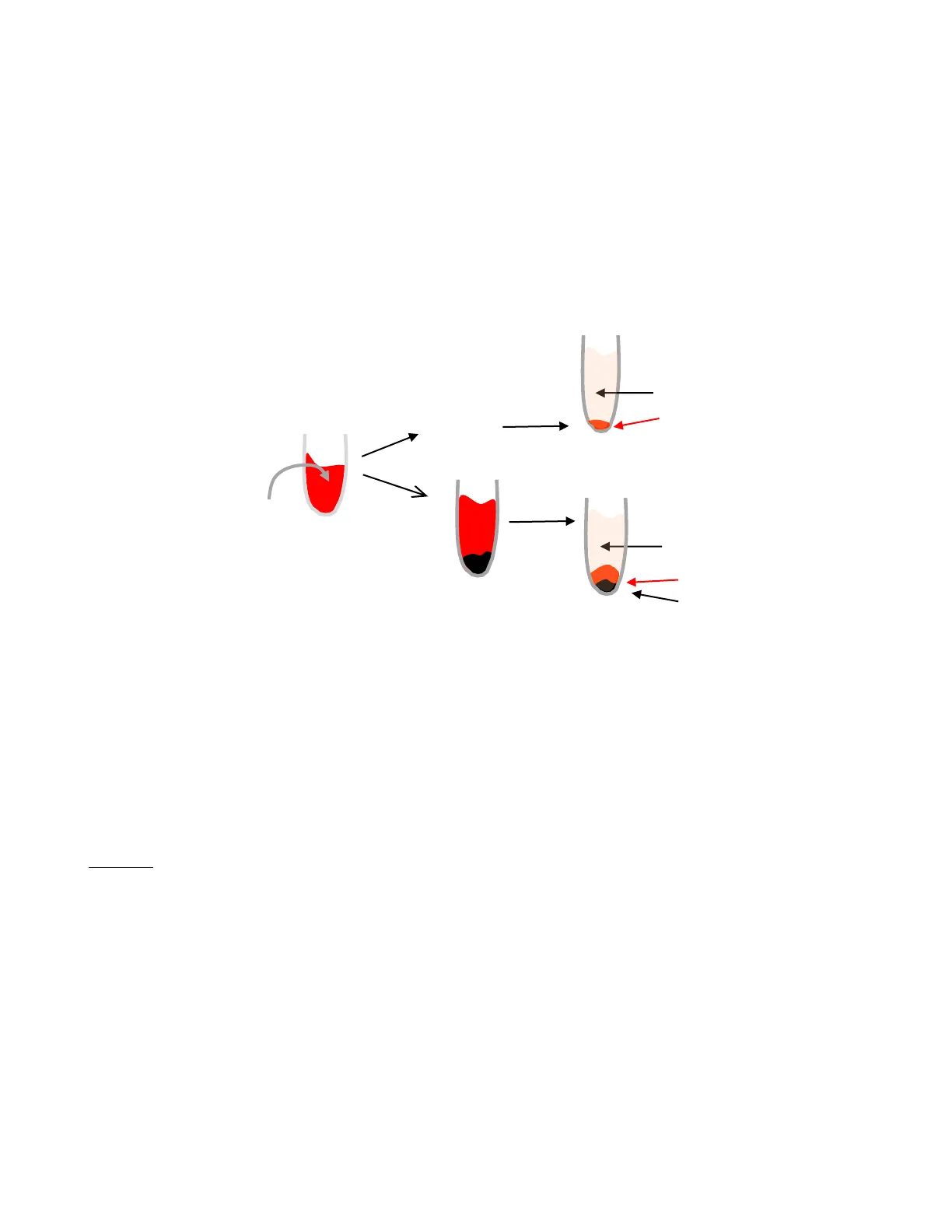
CAPILLARY Increased plasma levels of intracellular enzymes due to cell damage Enzymes A Normal cell turnover B Cell necrosis as a result of disease or trauma Copyright @ 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cellular Organelle Functions
MITOCHONDRIA · TCA cycle . Fatty acid oxidation · Oxidation of pyruvate CYTOSOL · Glycolysis · HMP pathway . Fatty acid synthesis NUCLEUS . DNA and RNA synthesis LYSOSOME . Degradation of complex macromolecules Copyright 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins
Fluids Obtained from Blood Samples
Laboratory assays of enzyme activity most often use serum, prepared from blood from a patient. plasma - the fluid, non-cellular fraction of blood (physiological - plasma exists in our bodies) serum - fluid obtained by centrifugation of coagulated whole blood (a non-physiological fluid) Benefit to serum -blood has already clotted and does not require any additives to prevent clotting Drawback to serum - hemolysis (breakdown of red blood cells) may occur before cells are separated out. These lysed red blood cells release enzymes and may cause false positive tests.
Reasons for Enzyme Appearance in Blood Plasma
PLASMA Add an anticoagulant. centrifuge Blood cells Patient's Blood Sample centrifuge Add nothing; allow clot to form. SERUM clot - Blood cells Clot Because cells of different tissues/organs contain different types of enzymes it is often possible to determine where damage (from disease processes, in response to drug therapies, from injury etc.) has occurred by observing the types of enzymes in the blood.
Enzyme Levels in Health and Pathology
- In health Basal (normal background) levels of enzymes in the plasma are usually due to normal cell turnover.
- In pathology (disease) Increased blood plasma enzyme levels (greater than basal levels) may result from:
- Cell membrane injury (such as in hepatitis, myocardial infarction)
- Enzyme induction (such as in response to metabolism of certain drugs)
- Tumor
- Cell proliferation (such as in bone healing)
Some enzymes have high activity in only one or a few tissues. The presence of increased levels of these enzymes in plasma reflects damage to the corresponding tissue. Increases in plasma levels of enzymes with a wide tissue distribution provide a less specific indication of the site of cellular injury. 2
Chemistry Profiles
Commonly Measured Enzymes
| enzyme | abbreviation(s) | tissue/organ source |
| alkaline phosphatase | ALP or ALK | liver, bone osteoblasts |
| gamma glutamyl transferase | GGT or GGTP | liver, pancreas |
| transaminases: | ||
| alanine aminotransferase | ALT or SGPT | liver |
| (serum glutamate-pyruvate transaminase) | ||
| aspartate aminotransferase | AST or SGOT | liver, muscle |
| (serum glutamate-oxaloacetate transaminase) | ||
| lactate dehydrogenase | LDH or LD | liver, muscle, erythrocytes |
| creatine kinase | CK or CPK | muscle |
Sample Profile Data
| TEST | COLLECTED 10/17/24 0630 | 10/19/24 0645 | UNITS | REF RANGE |
| GLUCOSE | 86 | 82 | MG/DL | 70-100 |
| BUN | 29 H | 13 | MG/DL | 9-22 |
| CREAT | 0.6 L | 0.7 | MG/DL | 0.7-1.5 |
| B/C | 48 H | 19 | MG/DL | 10-20 |
| URIC ACID | 3.1 L | 3.0 L | MG/DL | 3.9-9.0 |
| PO4 | 2.7 | 1.1 L | MG/DL | 2.5-4.5 |
| CALCIUM | 8.1 L | 8.9 | MG/DL | 8.5-10.5 |
| NA | 143 | 140 | MEQ/L | 138-148 |
| K | 4.0 | 3.8 | MEQ/L | 3.5-5.0 |
| Cl | 110 | 102 | MEQ/L | 100-112 |
| CO2 | 20 L | 18 L | MEQ/L | 23-39 |
| EBAL | 17 | 24 H | MEQ/L | 8-20 |
| TRIG | 261 H | 263 H | MG/DL | 1-160 |
| CHOL | 150 | 152 | MG/DL | 140-200 |
| BILLI - T | 30.4 H | 32.6 H | MG/DL | 0.2-1.0 |
| BILLI - D | 16.3 H | 17.7 H | MG/DL | 0.0-0.4 |
| BILLI - I | 14.1 H | 14.9 H | MG/DL | 0.0-1.2 |
| ALK | 99 | 100 | U/L | 30-101 |
| GGT | 223 H | 187 H | U/L | 9-38 |
| SGPT | 108 H | 136 H | U/L | 0-45 |
| SGOT | 309 H | 339 H | U/L | 0-40 |
| LDH | 345 H | 339 H | U/L | 60-230 |
| CPK | 688 H | 614 H | U/L | 0-255 |
| IRON | 211 | 231 H | MCG/DL | 60-230 |
| PROTEIN | 7.1 | 6.9 | G/DL | 6.0-8.0 |
| ALBUMIN | 3.5 | 3.2 L | G/DL | 3.5-5.5 |
| GLOBULIN | 3.6 | 3.9 | G/DL | 2.0-4.0 |
| A/G | 1.0 | 0.9 | G/DL | 0.6-2.4 |
3 e g
Basic Metabolic Panel (BMP)
A group of 8 tests standardized in the USA.
- Glucose
- Calcium
- Sodium
- Potassium
- CO2
- Chloride
- BUN
- Creatinine
Comprehensive Metabolic Panel (CMP)
A group of 14 tests standardized in the USA.
- Glucose
- Chloride
- Calcium
- BUN
- Albumin
- Creatinine
- Total Protein
- ALP (alkaline phosphatase)
- Sodium
- ALT (alanine aminotransferase)
- Potassium
- AST (aspartate aminotransferase)
- CO2
- Bilirubin
Organ Profiles
Renal Profile Muscle Profile Liver Profile See also Table 5.2 in LIR Biochemistry, 8th edition (page 70). Some other enzymes may be measured routinely. Amylase and lipase are enzymes that originate in the pancreas. 5'-NT can assess hepatobiliary disease. Acid phosphatase (PSA) is often ordered to assess the prostate. When used in conjunction with a patient's medical history and physical examination, such profiles can aid in the diagnosis of pathology. They may also be used to follow a patient's response to treatment, to indicate whether there is an adverse effect to a drug therapy, as well as to make a prognosis. 4
Liver Function Tests (LFTs)
For patients with liver disease, tests in the liver profile may be within or outside reference ranges depending on the cause or type of damage in the liver. Many disease processes have very distinct abnormalities in the liver enzymes. In addition to enzyme levels, liver function tests can include measurements of albumin and blood clotting (e.g. tests including the PT and INR) because albumin and clotting enzymes are produced in the liver, as well as bilirubin which is processed in the liver. Ratios of ALP to ALT and AST to ALT can be informative: A greater than 10-fold increase in ALT and a less than 3-fold increase in ALP suggests the injury is hepatocellular.
Alcohol-Induced Liver Damage
- Alcohol In patients with alcohol use disorder, the AST to ALT ratio is generally at least 2:1 Elevated GGT, along with AST, also suggests alcohol-induced liver damage. GGT should not be used alone since it is not very specific for alcohol.
Cholestasis (Bile Duct Blockage)
- Cholestasis (bile duct blockage) An increase in ALP compared to ALT and AST, suggests biliary obstruction. GGT is usually also elevated in cholestasis.
- A less than 10-fold increase in ALT and a more than 3-fold increase in ALP suggests cholestasis.
Drug-Induced Liver Damage
- Drugs Several medications are known to cause liver damage, including acetaminophen, NSAIDs, some antibiotics, statins, certain anti-seizure drugs, drugs for tuberculosis treatment, and some herbal medications.
Fatty Liver Disease
- Fatty liver disease (nonalcoholic steatohepatitis) AST and ALT are usually both elevated with a ratio of 1:1, with other liver function tests being normal.
Hepatitis Types
- Hepatitis
Viral Hepatitis
a. Viral - ALT and AST levels may be 20-50 times higher than normal, with some cases exceeding 10,000 U/L Viral hepatitis B, C, and D can cause chronic hepatitis, while hepatitis A and E cause acute viral hepatitis. Several other viruses, including HIV, Epstein-Barr (EBV), and Cytomegalovirus (CMV), can also cause hepatitis.
Autoimmune Hepatitis
b. Autoimmune Autoimmune hepatitis is a chronic disease characterized by continuing hepatocellular inflammation, necrosis, and a tendency to progress to cirrhosis. Patients usually have high LFTs without apparent cause. These patients may have positive tests for autoantibodies. 5 e g 5
Test Results for Healthy Individuals
Establishment of Reference Ranges
Gaussian Distributions
- Gaussian distributions For most tests in the chemistry profile, results for the normal, healthy population will show a Gaussian distribution (bell-shaped curve).
< 1 S.D. 1 S.D.> 2 S.D. S.D. 0.15% 14% 33.5% 33.5% 14% 2.33% 15% 3 S.D. S MEAN The mean and standard deviation of each analyte are first calculated from the results obtained by the normal, healthy group that is sampled. The Gaussian distribution of results is such that: 67% of normal, healthy individuals will give a result within 1 standard deviation of the mean (i.e., mean + 1 S.D.) 95% of normal, healthy individuals will give a result within 2 standard deviations of the mean (i.e., mean + 2 S.D.) 99.7% of normal, healthy individuals will give a result with 3 standard deviations of the mean (i.e., mean + 3 S.D.) Most reference ranges are established using the mean + 2 standard deviations of the mean. Given that the normal range for AST/SGOT is 0-40 mg/dl (0-40 = mean + 2 S.D.) What are the mean and the standard deviation for AST/SGOT in the normal, healthy population? What percentage of normal, healthy individuals will have an AST/SGOT result that is: A. Within reference range? B. Greater than reference range? C. Less than reference range?