The Human Reproductive System: Anatomy and Cycles
Slides from High school about Reproductive System. The Pdf details the human reproductive system, distinguishing between its male and female components, and outlining its four main functions. It includes an interactive activity for anatomical identification and a detailed explanation of the menstrual and ovarian cycles, suitable for Biology students.
See more28 Pages
Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Reproductive System Overview
Patricia Ripoll Reproductive System C O The Male and Female Reproductive Systems O
- The Human Reproductive System
It has four specific functions: To produce gametes (egg and sperm cells) To store and transport these reproductive cells To nurture offspring as it develops To produce hormones
Sexual Reproduction and Fertilization
Reproducción sexual Sexual reproduction Fecundación Fertilization https://www.youtube.com/watch? v=A645322ltak Espermatozoide (producido en los testículos) Sperm (produced in the testicles) + Óvulo (producido en los ovarios) Egg (produced in the ovaries) Útero Cigoto (en las trompas de falopio) Desarrollo embrionario (en el útero, hasta la 8 semana) Embryonic development (in the uterus, up to 8 weeks) Desarrollo fetal (en el útero, desde la 9 semana hasta el nacimiento) Fetal development (in utero, from 9 weeks to birth) Nacimiento - Infancia (hasta los 6 años) Birth - Childhood (up to 6 years) Niñez (6-10 años)- Preadolescencia (10-14 años) Childhood (6-10 years)- Preadolescence (10-14 years) Adolescencia (14-19 años)- Juventud (14-26 años) Adolescence (14-19 years)- Youth (14-26 years) Adultez (27-59 años)- Vejez (60 años o más) Adulthood (27-59 years) - Old age (60 years or more)
Physical Changes During Adolescence
Male Adolescent Changes
Phisical changes during adolescense Male
- Voice deepens.
- Muscular development.
- Ejaculation begins to occur.
- Facial and body (armpits, groin ... ) hair grows.
- Genitals develop and mature.
- PUBERTY.
Female Adolescent Changes
Female
- Mammary glands develop. Greater adipose tissue volume. Menstruation begins.
-
Facial and body (armpits, groin ... ) hair grows. Genitals develop and mature
Sex, Gender, or Sexuality?
SEX, GENDER OR SEXUALITY?
Gender and Social Behavior
Gender Social behaviour depending on your sex.
Affectionate Bonds and Feelings
Affectionate bonds Feelings you have for different people.
-
? Eroticism Related to sensual love and sexual desire.
Sexual Identity and Orientation
XXX Sexual identity Biological category in which you are identified. Sexual Orientation Related to which people you have feelings for. Cle
Sex: Genetically Determined Category
Sex Genetically determined biological category.
Male Reproductive Organs
Vas Deferens Function
Male Reproductive Organs Vas deferens Carries sperm from the testes to the urethra during ejaculation.
Testicles: Production and Hormones
Testicles
-
Production of male gamets (sperm).
- They are about 3℃ lower tan body temperature. Formed of million of seminiferous tubules, finishing in the epididymis.
- Finally conected to vas deferens. They produce hormones (testosterone)
Prostate Gland
Bladder Cowper's glands Prostate Underneath the bladder, surrounding the urethra. Produces prostatic fluid that activates the sperm and neutralise the acidity of female mucous secretions.
-
Connects ejaculatory duct with urethra.
Scrotum, Penis, and Urethra
Scrotum Penis Urethra Passageway for both urine and semen when exiting the body Used for both the elimination of urine from the body and the delivery of sperm for sexual reproduction. Composed of erectile tissue, Corpus spongiosum (Covers and protects the urethra) and Corpora cavernosa (Fill with blood during erection).
Male Reproductive System Components
Genital Tract Location
Male Reproductive System Genital tract Location Vas deferens From epididimys, to seminal vesicles. Epididymis Coiled tube attached to the top of each testicle Urethra From prostate, to outside.
Accessory Glands
Accesory Location glands Seminal vesicles Produce the seminal fluid. Prostate Produce the prostatic fluid. Cowper's glands Produce lubricating fluid before ejaculation.
Spermatogonia and Leydig Cells
Male Reproductive System testis Leydig cell Sertoli cell epididymis seminiferous tubules SPERMATOGONIA SPERM Each testicle is made up of millions of seminiferous tubules. The walls of the seminiferous tubules contain spermatogonia, which are cells will become male gametes (sperm). Sertoli cells nourish and support developing sperm cells. In the connective tissue that surrounds the seminiferous tubule we find the interstitial cells (also known as Leydig cells), which secrete testosterone into the blood.
Spermatogenesis: Sperm Formation
Spermatogenesis Formation of male gametes (sperm) https://www.youtube.co m/watch?v=h- IbOAG059c Head Occurs in the walls of the seminiferous tubules. This process begins when a boy reaches puberty. The beginning of puberty is marked by a boy's first ejaculation or spermarche. From that moment on, the testicles produce sperm continuously. However, testicular activity decreases, generally with age, as testosterone levels decrease. This process is called andropause. Acrosome: helps the sperm enter outer layer of the egg Mitochondrion: give energy to the sperm cell ... Middle piece Tail: give movement to the sperm cell ‹ ..................
The Journey of the Sperm Cell
The Journey of the Sperm Cell Semen: Liquid composed by prostatic fluid, sperms and is expel through the urethra. Sperm cells pass through different parts before reaching an egg cell to fertilise.
- Testes
Produce sperm
- Epididymis
Allows sperm to mature
- Vas deferens
Fallopian Tubes 8 Fertilisation Uterus 7 Cervix 6 Vagina 5 4 Urethra Where mixing of fluids occur
Cowper's glands: Help to lubricate the urethra and neutralize acidity before ejaculation, facilitating the passage of sperm. Ejaculation
Female Reproductive Organs
Fallopian Tubes and Fertilization
Female Reproductive Organs Fallopian Tubes
- Tubes that connect to the ovaries by a wider section called the infundibulum.
- Here is where, if it takes place, the fertilisation occurs.
- Finally connected to the uterus.
Uterus: Implantation and Growth
Uterus
- Where a fertilised egg implants and grows into a fetus during pregnancy. Walls made of a thick layer of smooth muscle called myometrium. Internally covered by a endometrium, with many blood vessels.
Cervix Function
Cervix Allows menstrual blood to flow from the uterus and serves as a pathway for sperm to enter the uterus.
Ovary: Egg and Hormone Production
Ovary Production of female gamets (egg).
- Suspended by small ligaments.
- Formed of medulla (inner part) and cortex (outer part).
- Cortex with follicles that produce eggs. They produce hormones (oestrogens and progesterone).
Vagina: Reproduction and Childbirth
Vagina
-
Receives the penis during sexual reproduction, allows the menstrual blood to exit the body, and lets the baby passes through during childbirth.
- The opening is partially covered by a membrane called hymen.
Female Reproductive System Components
Gonads: Ovaries
S Female Reproductive System Gonads They are the glands that have the function of providing genital differentiation between human beings Ovaries
Genital Tract Organs
Genital tract Organs of the reproductive system
-
Fallopian tubes
-
Uterus Vagina
External Genitalia
External genitalia Vulva
-
Clitoris 0
Oogenesis: Formation of Female Gametes
https://www.youtube.com/wa tch?v=b8qxYjT6iAk Oogenesis Formation of female gametes (eggs) Inside the follicles. Each follicle contains an oocyte that matures to become an egg. Oogenesis starts when girls reach menarche (their first period) during adolescence. It continues until the menopause, when the ovaries stop working. Oocytes mature to become eggs in a cyclical process called the ovarian cycle. Typically, the two ovaries alternate in releasing an egg each month. Follicles with immature oocytes inside Blood vessels Corpus luteum Follicle with a mature oocyte inside The mature oocyte exists the ovary
Egg Cell Structure
XXX Egg Cell Immature follicles Oocytes in developing follicles Egg C Follicle ruptures Nucleus: Contain 23 chromosomes (half). Zona pellucida Protective membrane in the middle. Corona radiata: Protective outside membrane with follicular cells that nourish the egg. Vitelline membrane: Inner protective membrane.
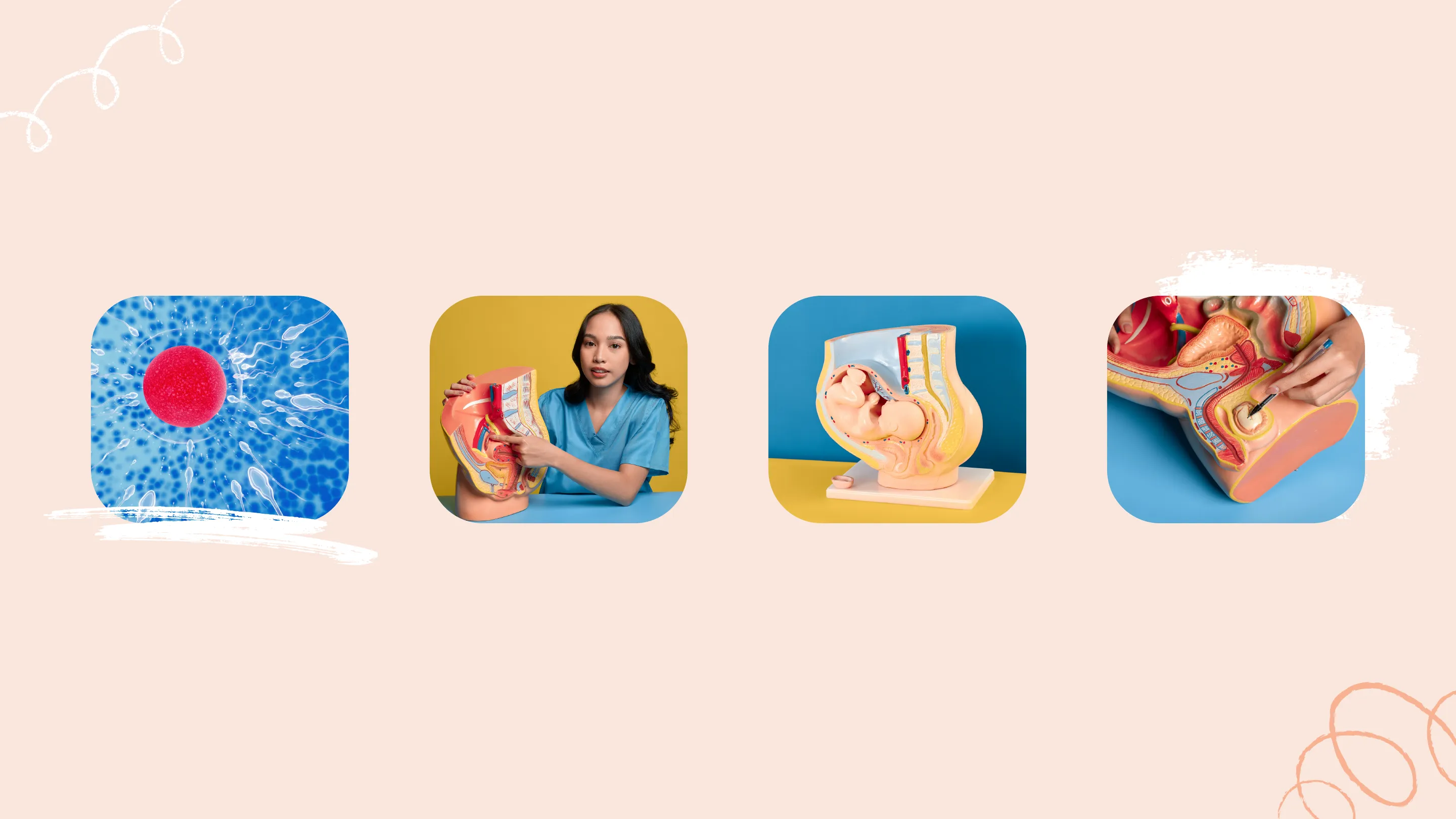
Puzzle Time: Identifying Reproductive System Parts
Puzzle Time! Let's try correctly identifying all the parts of the male and female reproductive systems. A ? D - . B C E F G H J IANSWER KEY Puzzle Time! Vas deferens Oviduct Ovary Urethra Prostate Uterus Vagina Testes Penis Cervix
Menstrual and Ovarian Cycle
Menstrual and Ovarian Cycle The ovarian and menstrual cycles are linked. They starts at puberty, so the oocytes can continue their development and the uterus can get ready for a possible pregnancy. They are both regulated by hormones. They occur approximately every 28 days if no fertilization has occurred.
-
Ovarian cycle: set of changes that occur in the ovary so that the oocyte can mature and the egg can be produced and released from the ovary.
-
Menstrual cycle: set of changes that occur in the endometrium of the uterus to prepare it for implantation of the embryo.
xxx Ix. X' X' X' X' X' XXX
Stages of the Ovarian Cycle
Menstruation Phase
Menstruation Lining of the uterus is shed, resulting in the release of blood and tissue from the body through the vagina.
Luteal Phase
Luteal Phase If fertilisation has not taken place, on day 28 the woman starts her period. The broken follicle transforms to become the corpus luteum. LH stimulates the corpus luteum to secrete progesterone.
1 5 6 7 8 2 1 28 11 27 12 26 13 25 14 24 15 23 16 22 17 21 18 20 19
Follicular Phase
Follicular Phase The pituitary gland produces FSH (follicle- stimulating hormone), which stimulates the ovaries, resulting in the maturation of a follicle and the oocyte it contains. 9 As the follicle grows, it starts to produce oestrogens.
Ovulation Phase
10 Ovulation Phase Levels of FSH and oestrogens are at their highest. The pituitary gland starts to release LH (luteinising hormone), causing the mature follicle to rupture and release an egg into the fallopian tubes. Woman is fertile. Stages of the Ovarian Cycle 4 3
Menstrual Cycle Phases
Menstruation: First Day of Cycle
Menstrual Cycle Menstruation: Starts on the first day of the cycle and lasts between five and seven days.
- If fertilization has not taken place during the previous cycle, the corpus luteum breaks down in the ovary and stops producing progesterone. This causes the endometrium to break away from the uterus and the woman has a period. The endometrium comes out dragging the oocyte.
-
If fertilization has taken place, the embryo will produce a hormone very similar to LH so that the corpus luteum can still produces more hormones. In this case, there won't be a period (or menstruation). The oocyte is fertilized and finish oogenesis.
Proliferative Phase
Proliferative Phase: Begins when menstruation ends and lasts until ovulation. The oestrogens produced by the ovarian follicle stimulate the endometrium in the uterus, causing it to thicken and increase the number of blood vessels. 77777
Secretory Phase
Secretory Phase: Starts after ovulation and continues until the start of the next period. Progesterone secreted by the corpus luteum causes maximum thickening of the endometrium, preparing it for possible implantation of a fertilized egg. leeX
Menstrual and Ovarian Cycle Hormones
Menstrual and Ovarian Cycle 1 2 3 O Ovarian cycle Follicle matures Follicle released Corpus luteum breaks down FSH Oestradiol (oestrogen) Menstruation br period Ovulation Endometrium thickens LH Progesterone Menstrual cycle 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 Days A B C I