Communication Skills in Medical Context: Patient Education and Decision Making
Document about Communication Skills – 4th Year. The Pdf explores communication skills in the medical field, focusing on patient education and decision-making. It covers disease-centered and patient-centered models, strategies for effective communication, and error management in medical practice for university students.
See more29 Pages
Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Patient Education
"Any set of planned learning opportunities offered to patients to enhance the knowledge of their disease and the ability to manage and cope with it".
"Its aim is to help patients and their families to understand the disease and the treatment, cooperate with healthcare providers, manage their own health, and maintain and/or improve their quality of life."
Patient education is important especially in chronic diseases. It's important because:
- Chronic diseases are treatable but not curable (asthma, T2D, HTN, HIV, Crohn's, Alzheimers)
- They have psychological consequences (anxiety, stress, loss, change in body image, self-identity)
- They go through the 5 stages of grief (denial, anger, bargaining, depression, acceptance)
> W chronic disease, you will make long-lasting relationships w your patients. > Patients become experts and have to take care of themselves > Chronic diseases highlight the connections between the medical and psychosocial dimensions > Shift from cure to patient education (promote self-management and empowerment; diminish complications and enhance QoL)
The 1st patient education program reduced hospital days from 5.4 to 1.7days. Preventable admissions, as diabetic coma reduced by 2/3 and cost savings of $1.7-3.4 mil. For the first time in the history of medicine it was proven on a large scale that the patient's education played a therapeutic role of prime importance.
It is a integral part of treatment and care v It is a continuous process, which has to be adapted to the course of the disease and to the patient's adaptation process V It is patient-centered: it concerns the patient's daily life and psychosocial enviro / It engages the patient's family/friends. V It uses a combination of methods (one-to-one or group interventions, teaching, counselling and behaviour modification techniques) ( It is multi-professional
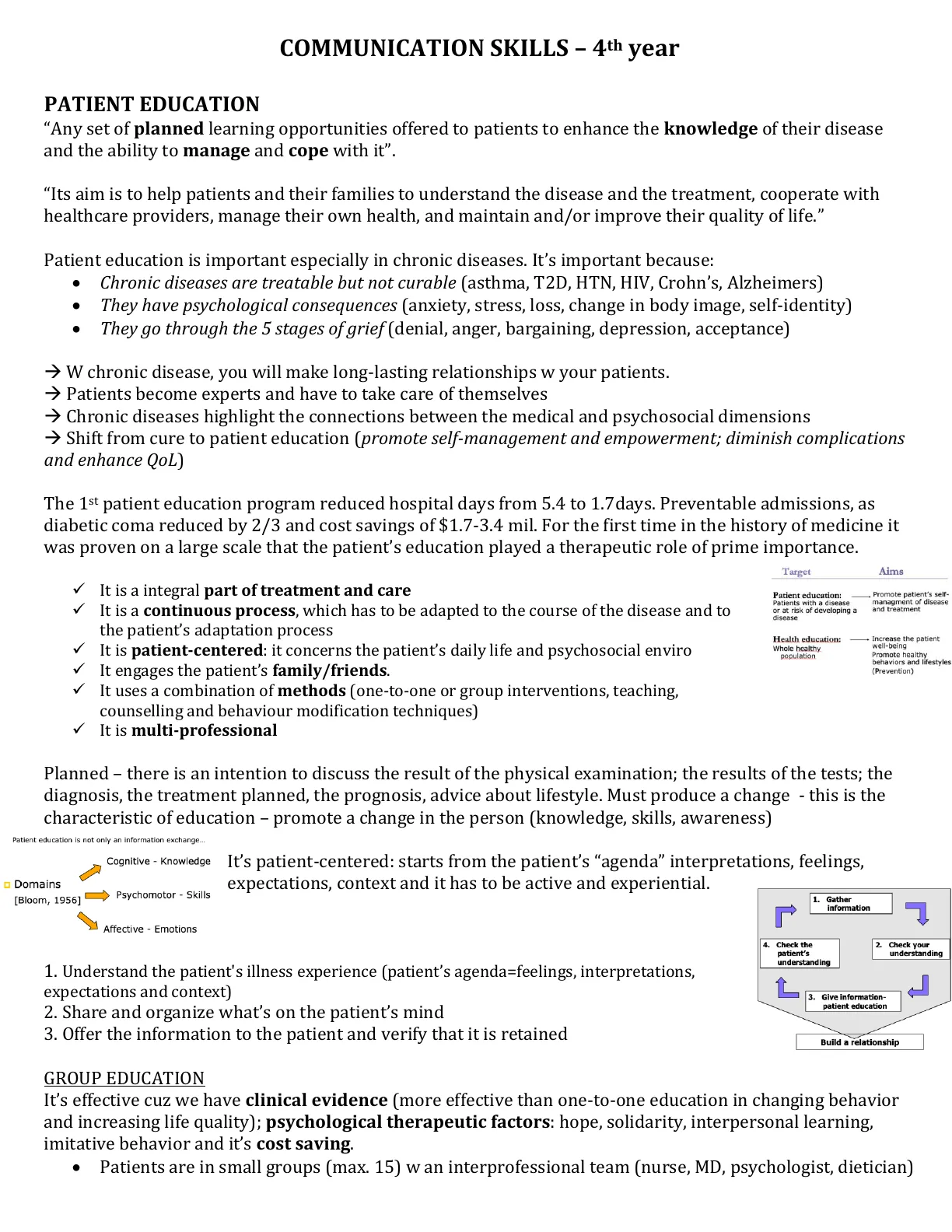
Patient Education vs. Health Education
Target Aims Patient education: Patients with a disease or at risk of developing a disease Promote patient's self- managment of disease and treatment Health education: Whole healthy population Increase the patient well-being Promote healthy behaviors and lifestyles (Prevention)
Planned - there is an intention to discuss the result of the physical examination; the results of the tests; the diagnosis, the treatment planned, the prognosis, advice about lifestyle. Must produce a change - this is the characteristic of education - promote a change in the person (knowledge, skills, awareness)
Patient education is not only an information exchange ...
Cognitive - Knowledge It's patient-centered: starts from the patient's "agenda" interpretations, feelings, Psychomotor - Skills expectations, context and it has to be active and experiential. Affective - Emotions
- Understand the patient's illness experience (patient's agenda=feelings, interpretations, expectations and context)
- Share and organize what's on the patient's mind
- Offer the information to the patient and verify that it is retained
1. Gather information L 7 4. Check the patient's understanding 2. Check your understanding 7 3. Give information- patient education Build a relationship
Group Education
It's effective cuz we have clinical evidence (more effective than one-to-one education in changing behavior and increasing life quality); psychological therapeutic factors: hope, solidarity, interpersonal learning, imitative behavior and it's cost saving.
- Patients are in small groups (max. 15) w an interprofessional team (nurse, MD, psychologist, dietician) o Domains [Bloom, 1956]
Judgment and Decision Making
A lot of decisions constantly taken by physicians: info to collect, diagnosis, treatment, prognosis. Decisions are complex, vulnerable to errors at multiple levels.
A lot of decisions constantly taken by patients too: if/when to go to a physician, info to report, trust what they've been told, compliance to the proposed treatment.
In evaluating a patient, the doctor must estimate:
- The probability of a number of possible hypotheses (i.e. diagnoses)
- Decide what additional information to gather in order to rule out all but one diagnosis
- Test competing hypotheses by evaluating the information that has been gathered. In actual practice, of course, these processes occur more or less concurrently as each step provides feedback for the others.
"Errors related to diagnosis were consistently noted to be the most common category across all studies, varying from 26 to 78% of identified errors. The 2nd most common category of error type related to treatment, either delayed or inappropriate, varying from 11 to 42% of identified errors. Studies that tried to develop an understanding of the causes of error noted that the cause was often multiple and that in up to 50% no cause was identified. A third of the identified adverse events involved errors of execution (slips, lapses, or oversights in carrying out appropriate management in correctly diagnosed patients), but almost half involved errors of reasoning or decision quality (failure to elicit, synthesize, decide, or act on clinical info). Such reasoning errors led to death or permanent disability in at least 25% of cases, and at least 3/4 were deemed highly preventable. Most errors in clinical reasoning are not caused by incompetence or inadequate knowledge but due to the frailty of human thinking under conditions of complexity, uncertainty and pressure of time".
ERRORS in medical practice: Adverse events occurred in 3.7% of the hospitalizations and 27.5% of the adverse events were due to negligence > permanent disability or death.
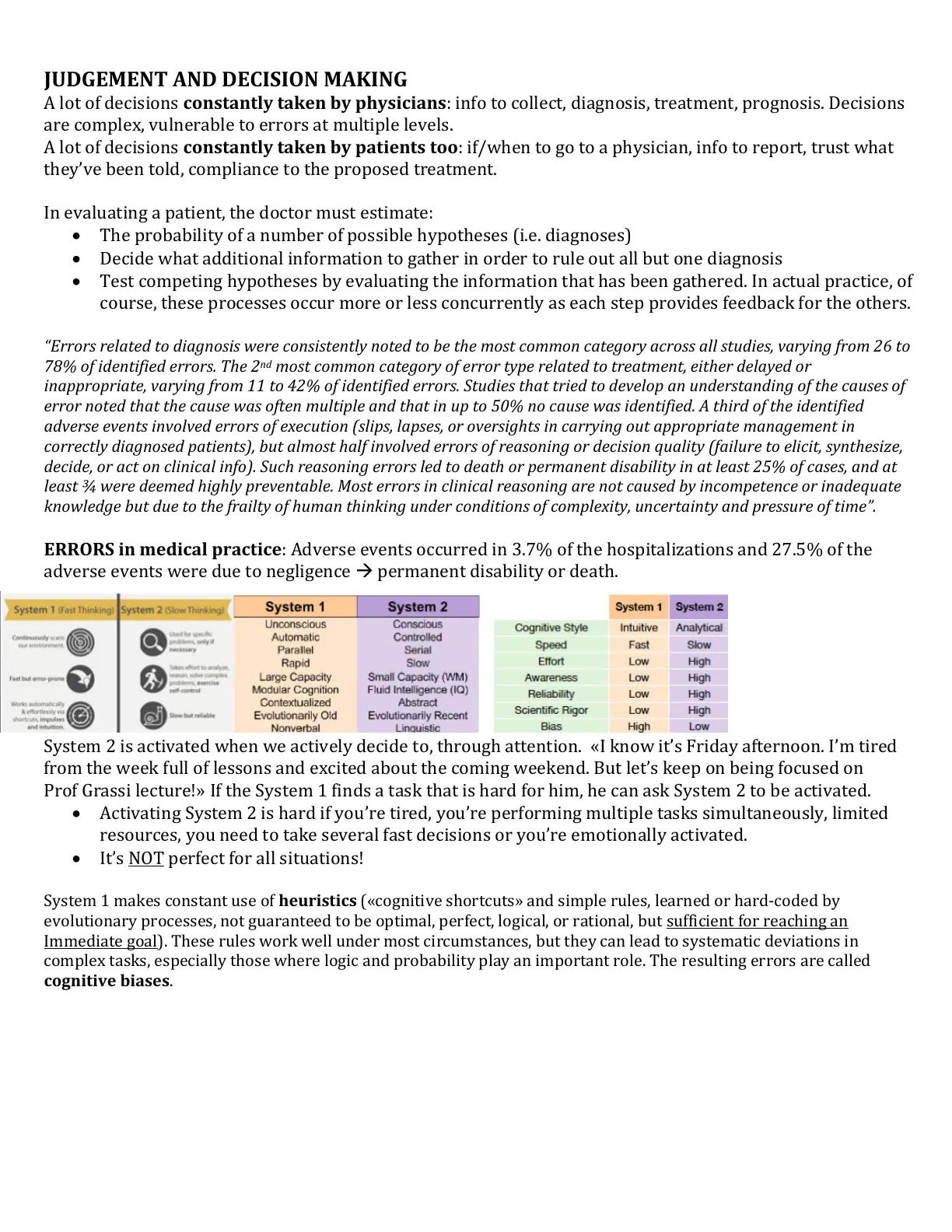
System 1 vs. System 2 Thinking
System 1 (Fast Thinking) System 2 (Slow Thinking) System 1 System 2 System 1 System 2 Unconscious Conscious Cognitive Style Intuitive Analytical Continuously scans our environment. Used for specific problems, only if necessary Automatic Parallel Rapid Controlled Serial Slow Speed Fast Slow Effort Low High Fast but error-prone Takes effort to analyze. mison solvy complex problems, exercise self-control Large Capacity Modular Cognition Contextualized Small Capacity (WM) Awareness Low High Reliability Low High Works automatically & effortlessly via shortcuts, impulses and intuition Slow but reliable Evolutionarily Old Nonverbal Evolutionarily Recent Linguistic Scientific Rigor Low High Bias High Low
System 2 is activated when we actively decide to, through attention. «I know it's Friday afternoon. I'm tired from the week full of lessons and excited about the coming weekend. But let's keep on being focused on Prof Grassi lecture!>> If the System 1 finds a task that is hard for him, he can ask System 2 to be activated.
- Activating System 2 is hard if you're tired, you're performing multiple tasks simultaneously, limited resources, you need to take several fast decisions or you're emotionally activated.
- It's NOT perfect for all situations!
System 1 makes constant use of heuristics («cognitive shortcuts» and simple rules, learned or hard-coded by evolutionary processes, not guaranteed to be optimal, perfect, logical, or rational, but sufficient for reaching an Immediate goal). These rules work well under most circumstances, but they can lead to systematic deviations in complex tasks, especially those where logic and probability play an important role. The resulting errors are called cognitive biases.
Fluid Intelligence (IQ) Abstract
Cognitive Biases: Anchoring Heuristic
ANCHORING HEURISTIC: Individuals use the initial piece of information they have to make subsequent judgments and decisions. Once the value of this anchor is set, all future negotiations, arguments, estimates, etc. are discussed in relation to the anchor.
- Diagnostic Process: Prematurely settling on a single diagnosis based on a few important features of the initial presentation or information. Failing to adjust as new information become available or prematurely stopping in a diagnostic process, accepting a diagnosis before gathering all the necessary information or exploring all the important alternatives (Premature Closure).
- W Patients: Patients may arrive to the physician with anchoring ideas about what they suffer from, what treatment they have to do, what their prognosis will be, etc. Pay also attention not to create early anchors in patients!
«Ok, It seems to be a simple flu from what you have told me by now. But please tell me also this o further information ... » o «The usual initial dosage is 100mg per day but given your condition I prescribe you 150mg»
Cognitive Biases: Availability Heuristic
AVAILABILITY HEURISTIC: The estimate of the probability of a certain event is based on the easiness to recall in mind examples of it. Such easiness is not only related to how often you saw it occurring but also how emotionally pregnant is the event and if you have personal experience of it.
- Deaths from strokes happen twice as often than deaths from any kind of accident, but 80% of people think dying from accidents is more probable.
- If you mainly work with patients with a certain disorder, you conduct researches on it, you were told a very dramatic story of a patient suffering from it, or a close relative died from it, you will tend to think that this disorder is more prevalent, and tend to over-diagnose it.
I'LL NEVER FLY AGAIN! THE DAILY TOUANRA 12 DIE IN AIRPLANE CRASH !!
Cognitive Biases: Base Rate Neglect or Representativeness Heuristic
BASE RATE NEGLECT OR REPRESENTATIVENESS HEURISTIC: We tend to estimate the probability of an event based on how it is a typical prototype of a class of events, neglecting the a priori probability of that class of events.
"You are a family doctor and your patient has a certain symptom. You know that people suffering from a very . rare disease have this symptom 100% of times. But also people suffering from another common disease may sometimes experience these symptoms, only 2% of times. If you only know this information, which is the most probable diagnosis? We do probabilities > the common disease!" But you'd think he has the rare disease ...
Cognitive Biases: Gambler's Fallacy
GAMBLER'S FALLACY: The erroneous belief that chance is self correcting, or that if something happens more frequently than normal during a given period, it will happen less frequently in the future or vice versa, even if the probability of every occurrence is totally independent from the past ones. "In the ER, one might diagnose 3 patients in a row with PE, and therefore believe that it is unlikely the next patient will also have a PE, despite the fact that the patients are clearly unrelated".
Cognitive Biases: Confirmation Bias
CONFIRMATION BIAS: It's actively gathering and selectively interpreting evidence that confirms a hypothesis and ignoring evidence that might disconfirm it.
- "A patient presents with a throbbing unilateral headache, photophobia, and nausea. I think she can have migraine. So I ask her about relatives and she actually has a family history of migraine. This further confirms my diagnostic hypothesis!» She also told you that she has what seems an onset of a thunderclap headache, but you did not take care of this piece of information and you did not actively look for information that can falsify the diagnostic hypothesis of migraine."
- «All swans are white» can be proven false looking for at least a single Black swan. Looking for further white swans does not help to discard it as false.
Cognitive Biases: Association-Causation
ASSOCIATION-CAUSATION: We are psychologically predisposed to think in causal terms when we have evidence of association. Causation is very hard to study and usually requires RCTs!
Possible interpretations: 1. Mediterranean diet causes a reduction in the risk of depression 2. Patients at risk of depression tend to like less Mediterranean diet food 3. There is a common cause (genes), which jointly predisposes to depression and to follow the Med. diet.