Nephrology: Renal Physiology and Associated Pathologies
Outlines from Medschoolbro about Nephrology. The Summaries cover renal embryology, anatomy, physiology, and various pathologies like nephrotic and nephritic syndromes, acid-base balance, and acute kidney injury. This University Biology material is ideal for students preparing for exams like the USMLE Step 1.
See more20 Pages
Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
NEPHROLOGY
MEDSCHOOLBRO"
Designed for you to pass USMLE Step 1
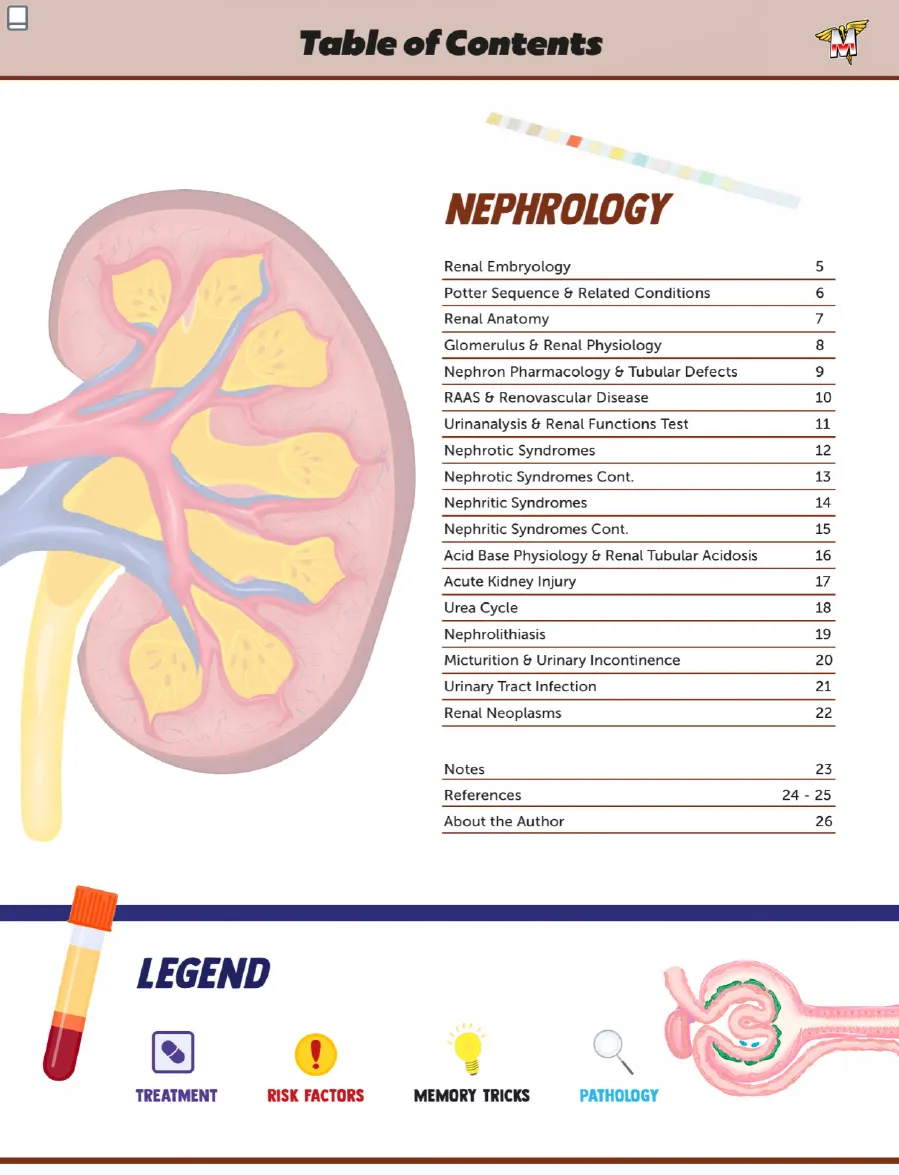
Table of Contents
NEPHROLOGY
Renal Embryology
5
Potter Sequence & Related Conditions
6
Renal Anatomy
7
Glomerulus & Renal Physiology
8
Nephron Pharmacology & Tubular Defects
9
RAAS & Renovascular Disease
10
Urinanalysis & Renal Functions Test
11
Nephrotic Syndromes
12
Nephrotic Syndromes Cont.
13
Nephritic Syndromes
14
Nephritic Syndromes Cont.
15
Acid Base Physiology & Renal Tubular Acidosis
16
Acute Kidney Injury
17
Urea Cycle
18
Nephrolithiasis
19
Micturition & Urinary Incontinence
20
Urinary Tract Infection
21
Renal Neoplasms
22
Notes
23
References
24 - 25
About the Author
26
LEGEND
- ! TREATMENT
- RISK FACTORS
- MEMORY TRICKS
- PATHOLOGY
Renal Embryology
PRONEPHROSMESONEPHROSMETANEPHROS
PRO -> MESO -> META = PROTOTYPE -> MIDDLEMAN->MATURE
Mesonephric Duct Development
PRONEPHROS = PROTOTYPE kidney
MESONEPHROS = MIDDLEMAN kidney
METANEPHROS = MATURE kidney
THINK! Renal Development Timing
PRO = 3 letters = week 3
MESO = 4 letters = week 4
Urogenital Sinus
PRONEPHROS
TEMPORARY
Forms in week 3 then
degenerates. A BLUEPRINT
for renal development.
MESONEPHROS
TEMPORARY
Appears in week 4, primary
secretory organ until week 9,
degenerates by week 12. Role in
male reproductive organs.
METANEPHROS
Arises in week 5, canalization
complete by week 10,
progresses to permanent
kidney by week 36 of gestation.
WEEKS of Kidney Development
1
2
3
4
5
6
7
8
9
10
11
12
METANEPHROS Formation
URETERIC BUD interacts with
METANEPHRIC MESENCHYME to become
mature kidney (aka METANEPHROS)!
Mesonephric (Wolffian) Duct
METANEPHRIC
MESENCHYME
Pelvis of
kidney
Kidney calyx
-7
URETERIC
BUD
THINK! Metanephric Mesenchyme Analogy
The Metanephric
mesenchyme are like a
plug connecting with the
uteric bud (socket!)
Metanephric Mesenchyme Structures
Glomerulus through
to the distal
convoluted tubule
Ureteric Bud Structures
Ureter
Pelvises
Calyces
Collecting ducts
! Malformed Kidneys
Dysfunctional/Abnormal
communication between
these embryological
structures can lead
to MALFORMED KIDNEYS
(i.e. Renal agenesis,
Dysplastic kidneys etc.)
METANEPHRIC MESENCHYME Characteristics
These structures
are mesodermal
structures!
URETERIC BUD Characteristics
- METANEPHROS
PERMANENT - Contact with bud
and mesenchyme
key for kidney
differentiation
URETEROPELVIC JUNCTION Obstruction
URETEROPELVIC JUNCTION is the
last to canalize which can
cause congenital obstruction.
This can be detected via
PRENATAL ULTRASOUND
Potter Sequence & Related Conditions
OLIGOHYDRAMNIOS Effects
REDUCED CUSHIONING FOR
THE DEVELOPING FETUS
COMPRESSION/TWISTING
OF DEVELOPING FETUS
POTTER Sequence
THINK! Babies who can't Pee develop POTTER Sequence
Bilateral RENAL
AGENESIS or bilateral
MULTICYSTIC
DYSPLASTIC KIDNEYS
Reduced fetal urine
excretion
Oligohydramnios
causing fetal
compression
POTTER Sequence Symptoms
P ulmonary hypoplasia
O ligohydramnios
T wisted face (Flattened nose, low set ears, receding chin)
T wisted skin (wrinkling)
E xtremity defects (Bowed legs, club feet)
R enal failure
CAUSES of Renal Conditions
POLYCYSTIC KIDNEY DISEASE PRESENTS AS: Flank pain, hematuria, HTN, UTI & progressive renal failure
REMEMBER! "Polycystic Kidney" has 16 letters, Most PKD is a due to a defect on CHROMOSOME 16!
AUTOSOMAL DOMINANT Polycystic Kidney Disease
Multiple cysts in the renal cortex
& medulla. 85% due to PKD1
mutation, 15% due to PKD2
mutation.
HTN and CKD common.
ASSOCIATED WITH: Berry aneurysms,
hepatic cysts, MVP and diverticulosis
TREATMENT: ACEi
AUTOSOMAL RECESSIVE Polycystic Kidney Disease
Subtype that can cause POTTER
Sequence!
Cystic dilation of ducts which appears
during infancy.
MULTICYSTIC DYSPLASTIC KIDNEY
Abnormal interaction
between ureteric
bud and metanephric
mesenchyme
creating a cystic, non
functional kidney.
> Largely
non-hereditary &
unilateral, but bilateral
leads to POTTER
Sequence!
RENAL AGENESIS
Ureteric bud does
not develop
fails to differentiate
into metanephric
mesenchyme leading
to complete absence of
kidney & ureter.
CHRONIC PLACENTAL INSUFFICIENCY
Hydronephrosis
POSTERIOR URETHRAL VALVE
Dilated ureter
Urinary reflux
Tissue remnant
in the posterior
urethra leading
to obstruction of
urine outflow.
Most common
cause of bladder
outlet obstruction
in MALES.
Distended bladder
Urethra obstructed
by posterior
urethral membrane
· Diagnosed via.
U/S & Voiding
cystourethrogram.
Renal Anatomy
Adrenal
Aorta
Kidney
Renal Pelvis
1
Renal pelvis
Metanephros
Renal
pelvis
Ureter
POINTS OF URETHRAL OBSTRUCTION
1 Ureteropelvic junction
2 Pelvic inlet
3 Ureterovesical junction
! HORSESHOE KIDNEY
FAILURE TO ASCEND CAN BE DUE TO HORSESHOE KIDNEY
HORSESHOE KIDNEY
> Kidneys fail to ascend as
they get stuck under the
INFERIOR MESENTERIC ARTERY
-> Fusion of inferior poles
> Increased incidence of
UTI's, Hydronephrosis,
Renal stones, & Renal
Cancer
> Higher incidence in
chromosomal aneuploidy
(i.e. Turners, Trisomies 13,
18, 21)
URETER Blood Supply
Despite receiving roughly 20% of our
bodies entire cardiac output, the renal
medulla receives less blood flow than
the cortex making it prone to ischemia!
THINK! Ureter Course
"Water (URETERS) flows OVER the iliac & UNDER
the bridge (uterine artery or vas deferens)!"
URETER BLOOD SUPPLY Details
Renal artery
(PROXIMAL)
Gonadal artery
Aorta
MIDDLE
Common iliac artery
Internal iliac artery
- Superior vesical artery
Uterine artery
Middle rectal artery
Vaginal artery
- Inferior vesical artery *in males
RENAL BLOOD FLOW Pathway
1 Renal artery
2 Segmental artery
3 Interlobar artery
4 Arcuate artery - interlobular artery
NOT SHOWN ....:
5 Afferent arteriole
6 Glomerulus
7 Efferent arteriole
8 Vasa recta
9 Venous outflow
Left renal vein is Longer,
and receives additional
tributaries via the Left
gonadal and
suprarenal veins
Kidney Anatomical Location
Kidvvnd to their anatomical
location at T12-13 by week 9 of
gestation
Glomerulus & Renal Physiology
Renal Equations
RENAL CLEARANCE
Effective clearance of substance
(X) from plasma (Px) to urine (Ux).
x
If Cx < GFR: net tubular
reabsorption and/or not
freely filtered.
If Cx > GFR: net tubular
secretion of X.
If Cx = GFR: no net
secretion or reabsorption
EFFECTIVE RENAL PLASMA FLOW (eRPF)
Para-aminohippuric acid (PAH) can be
used to estimate eRPF.
The amount of PLASMA filtered by the blood.
eRFP = U
PAH
PAH
e GFR
Estimated ability for kidneys to filter.
NOTE:
Pregnancy is
associated with
increased GFR!
INULIN & GFR Estimation
Freely filtered
CYSTATIN C & GFR Estimation
CAN USE
CREATININE & GFR Estimation
Slightly overestimates
GFR since
creatinine is moderately
secreted by kidneys
FILTRATION FRACTION (FF)
Percentatge of plasma that is filtered.
Filtration fraction (FF) = GFR/RFP.
Normal range of FF is roughly 20%
Glomerular Filtration Barrier Components
MADE UP OF:
> Basement membrane
(TYPE IV COLLAGEN)
Podocyte foot processes
A
BBDO
FP FP
Glomerular Filtration Barrier Filters
FILTERS PLASMA BASED ON:
SIZE:
Endothelium prevents
molecules > 100 nm from
being filtered. Slits b/w the
podocytes and basement
membrane prevent entry of
molecules >50-60 nm.
CHARGE:
Layers of the Glomerulus are
all negativley charged which
prevent negatively charged
molecules (i.e. ALBUMIN) from
being filtered.
NSAIDS & Afferent Arteriole
MAIN AREA FOR FILTRATION
Prostaglandins
preferentially dilate
afferent arteriole
(1 RPF, 1 GFR, so no 4 FF)
PDA: Prostaglandins
Dilate Afferent
BLOOD Filtration
Bowman capsule
(parietal layer)
Bowman space
Podocytes
(visceral layer)
Basement membrane
Filtered
Excreted
Reabsorbed
Secreted
THINK! ACE Inhibitors
ACE: Angiotensin II
Constricts Efferent
EFFERENT ARTERIOLE Constriction
Angiotensin II
ACE INHIBITORS -OH preferentially constricts
efferent arteriole
(IRPF, 1 GFR, so TF)
CHANGES IN GLOMERULAR DYNAMICS
GFR
RPF
FF (GFR/RPF)
Afferent arteriole constriction
-
Efferent arteriole constriction
1
1
T plasma protein concentration
plasma protein concentration
1
-
8
Dehydration
->
THINK! Plasma Dynamics
PLASMA
AFFERENT ARTERIOLE
x V/P
= CPAH*
PAH*
Constriction of ureter
Nephron Pharmacology & Tubular Defects
* = RENAL TUBULAR DEFECTS
PROXIMAL CONVOLUTED TUBULE
HCO,
Na+
Ca2+
1
H2O
Acetazolamide
MOA: Carbonic anhydrase inhibitor
OTHER USES: Glaucoma, metabolic
alkalosis, altitude sickness
AEs: "Acid" azolamide causes acidosis, can
cause sulfa allergy
Fanconi Syndrome
Reabsorption defect in the PCT -> excretion of
AA's, glucose, HCO2 & PO,3- - > metabolic acidosis
Fanconi Flushes nutrients down the PCT drain!
CORTEX & MEDULLA
CORTEX
MEDULLA
DESCENDING LIMB
Mannitol
Na*
K*
2CI-
Osmotic diuretic (increases tubular fluid osmolarity)
MOA: Elevated intracranial pressure
AEs: Dehydration, contraindicated in CHF & anuria!
THICK ASCENDING LIMB
Loop Diuretics
I.E .: Furosemide, Bumetanide,
Torsemide
MOA: Inhibits Na+/K+/2Cl-
cotransporter -> disrupts
hypertonicity of medulla
AEs: Ototoxicity, hypocalcemia/
hypomagnesemia
Loops Loose Ca2+ ->
THINK! can precipitate calcium
oxalate stones!
Bartter Syndrome
Reabsorption defect in the thick
asc. loop -> metabolic alkalosis
Bartter's BF is Furosemide
because they are twins
DISTAL CONVOLUTED TUBULE
Thiazide Diuretics
I.E .: Hydrochlorothiazide,
chlorthalidone, metolazone
MOA: Inhibits NaCI reabsorption
-> decreases Ca2+ excretion
AEs: THINK! HyperGLUC
HyperGlycemia
HyperLipidemia
HyperUricemia
HyperCalcemia
Gitelman Syndrome
Reabsorption defect of NaCl in
DCT -> metabolic alkalosis
Gitel is a man whose
mistaken for Thai(azide)
COLLECTING DUCT
Na+
K+ Sparing Diuretics
K
H+
I.E .: Spironolactone, Eplerenone,
Amiloride, Triamterene
MOA; Aldosterone receptor
antagonists
OTHER USES:
· Spironolactone: anti-androgen,
hepatic ascites
> Amiloride: nephrogenic DI
AEs: Hyperkalemia
Liddle Syndrome
* Liddle Syndrome
Mutation causing decreased
Na+ channel degradation ->
Increases Na+ reabsorption in
collecting tubules
Liddle but Dominant ->
Autosomal Dominant
S.A.M.E. (SYNDROME OF APPARENT MINERALOCORTICOID EXCESS)
* S.A.M.E
(SYNDROME OF APPARENT
MINERALOCORTICOID
EXCESS)
Decreased conversion of cortisol
to cortisone -> increases cortisol
-> increases mineralocorticoid
receptor activity
TREATMENT: K+ sparing
diuretics or corticosteriods
Na+ & CI- Transport
Na+
CI-
Sugars
Amino acids
Na+
RAAS & Renovascular Disease
Afferent Arteriole
MACULA DENSA
Chemoreceptor lined cells in the distal
convoluted tuble
Detects changes in concentraction of
NaCl and secretes PROSTAGLANDINS
JUXTAGLOMERULAR CELLS
Baroreceptor lined cells around the
afferent arterioles
> Detects decreases in renal perfusion
pressure
SYMPATHETIC ACTIVATION
> Detects low systemic BP & releases
norepinephrine
GLOMERULUS
Efferent arteriole
AT Il also
R
C
R
R
R
R
R
R
R
R
RENIN Conversion
RENIN converts Angiotensinogen
in the liver to Angiotensin I
JUXTAGLOMERULAR CELLS Secretion
JUXTAGLOMERULAR CELLS
to secrete RENIN into the
blood stream
Angiotensin II Effects
Increases GFR via
vasoconstriction of the
EFFERENT ARTERIOLES
&
Increases Na+, HCO3;,
& H2O reabsorption at
the PCT
KIDNEYS
a-INTERCALATED CELLS
Increase in H+/ATPase >
Increases H+ secretion
EFFECT OF ANGIOTENSIN II ON:
Synthesis of :
ALDOSTERONE in the
ADRENAL GLANDS
PRINCIPAL CELLS
ADRENALS
Nat absorption/K+ secretion
(via ENaC) & Increased H20
reabsorption (via aquaporins)
Angiotensin II Receptors
Binds to receptors
AT II receptors in the
hypothalamus
Promotes ADH secretion
at the posterior pituitary
> increases thirst + H20
reabsorption
Renovascular Disease
O Most common cause of secondary hypertension in adults.
CAUSES of Renovascular Disease
MOSTLY CAUSED BY:
Long-standing atherosclerosis on the
proximal 1/3 of the renal artery
> Classically in elder males who smoke!
Fibromuscular dysplasia of the distal 2/3
of the renal artery/segmental branches
4 Classically in young-middle aged women!
Renovascular Disease Manifestations
CAN CAUSE:
UNILATERAL
STENOSIS
Asymmetric kidney size.
Venous sampling will
show increased renin
in affected kidney and
decreased in unaffected.
BILATERAL
STENOSIS
Sudden increase in
Creatinine following
administration of ACEi,
ARB, or renin inhibitor.
Decreased
renal
perfusion
Increase in
renin
Increase in
Angiotensin
HYPERTENSION
Angiography Findings
"String of beads" on angiography
Systemic Vasoconstriction
THESE 3
ALL ACTIVATE:
causes
systemic
vasoconstriction
leading to an
increase in BP!
Angiotensin I Conversion
Angiotensin I is then converted
to ANGIOTENSIN II (AT ID) via
ACE primarily in the vascular
endothelial cells of the lungs
HYPOTHALAMUS Role
BOTH
WILL
CAUSE
Proximal
convoluted
tubule