Respiratory Physiology, Spirometry, Diseases, and Tests by Prof. Coppola
Slides from Prof. Coppola about Respiratory Physiology, Spirometry, Diseases, Tests. The Pdf, a university-level document for Biology students, covers basic respiratory physiology, static and dynamic mechanics, compliance, and elastance, including their pathological implications.
See more23 Pages
Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Respiratory Physiology Overview
Respiratory System Diseases #3 - Prof. Coppola - Respiratory Physiology Page 1 of 23 Respiratory System Disease #3 Respiratory Physiology, Spirometry, Diseases, Tests Prof. Coppola - 18/11/2021 Ragosta R. - Sancilio A.
Respiratory Physiology Introduction
1. Respiratory physiology Today I propose respiratory physiopathology, on Outlines HEALTH SCIENCES the one hand, we just have a recap of respiratory physiology, very briefly we claim to mind the basic physiology concept of how our respiratory system work, and then we deal with respiratory function tests, which will be the basis of our evaluation of the lung, and as I said before independently of what will be your future in the health system, you will deal with respiratory test. You will ask some patient to perform spirometry, you will ask a consultant in respiratory medicine to evaluate your patient for example before admitting him to surgery or something like that, and you will have in your hand maybe some tests of respiratory function that you will evaluate.
Static Mechanics of the Respiratory System
This is the outline of today: we start with a very brief recap of respiratory physiology. Remember that the respiratory system is divided into two conditions, which is static when the systems are relaxed, and the static mechanic is due not only to the lungs of course but is due also to the cage, which is constituted of bones and cartilaginous tissue, and the muscle apparatus. All these elements determine the static of the respiratory system.
- Static Mechanics
- Spirometry
- Bronchoreversibility and bronchoconstriction
- Dynamic Mechanics
Inspiration and Expiration Mechanics
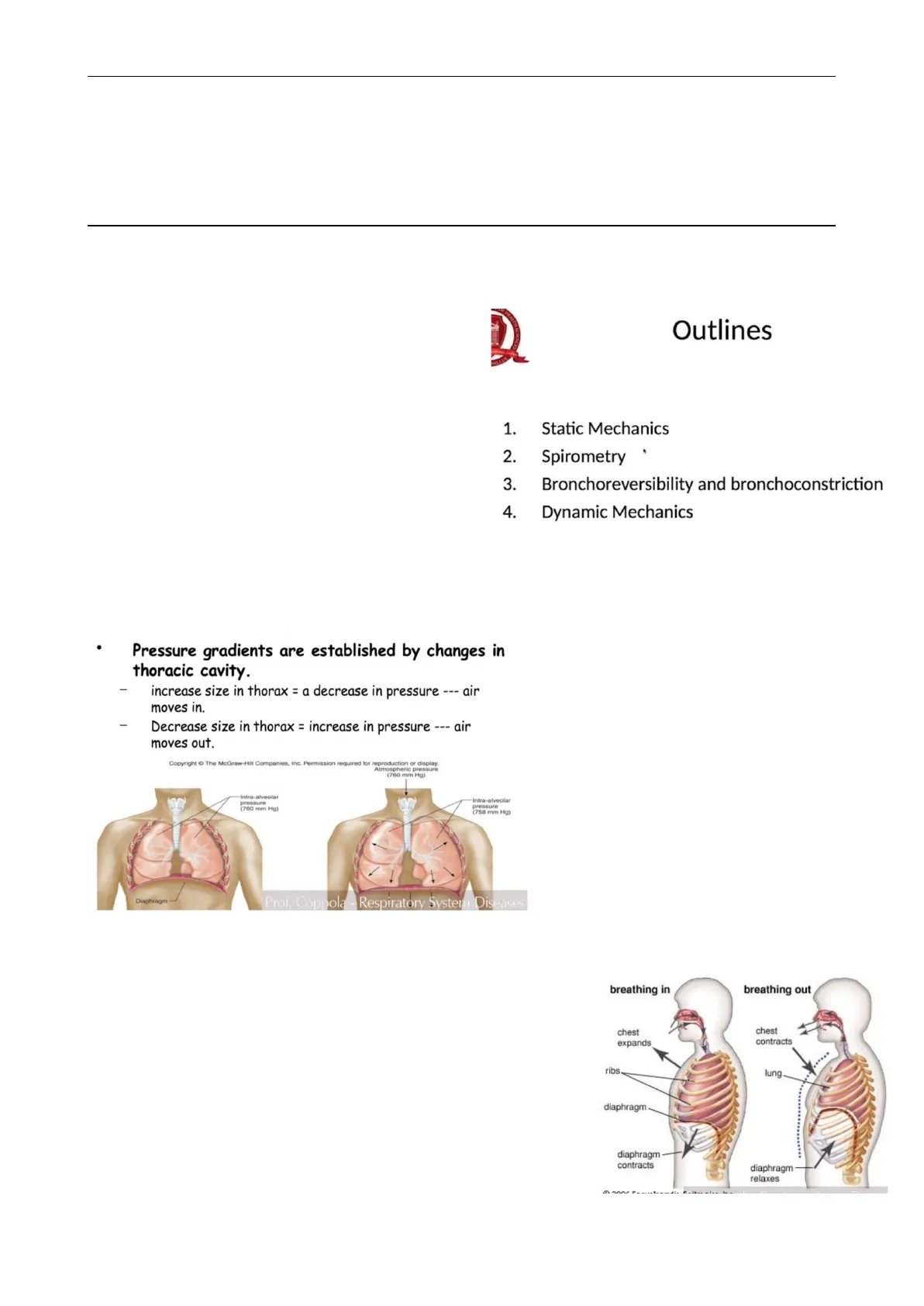
1.1 Inspiration and expiration According to that respiratory physiology take into account the static balance and the dynamic condition of the respiratory system. Very basically, inspiration and expiration depend on the variation of the volume of the thorax, the increased size of the thorax determines a decrease in pressure inside determinates of course the movement of air inside; and in the opposite, the decreasing size in thorax determinates an increase in pressure inside and produces expiration.
Pressure gradients are established by changes in thoracic cavity.
- increase size in thorax = a decrease in pressure --- air moves in.
- Decrease size in thorax = increase in pressure --- air moves out.
Copyright @ The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Atmospheric pressure (760 mm Hg) Intra-alveolar pressure (760 mm Hg) Intra-alveolar pressure (758 mm Hg) Diaphragm Prof. Coppola - Respiratory System Diseases breathing in breathing out chest expands chest contracts ribs lung diaphragm diaphragm contracts diaphragm relaxes Bonne Respiratory System Diseases #3 - Prof. Coppola - Respiratory Physiology Page 2 of 23
Active Inspiration Process
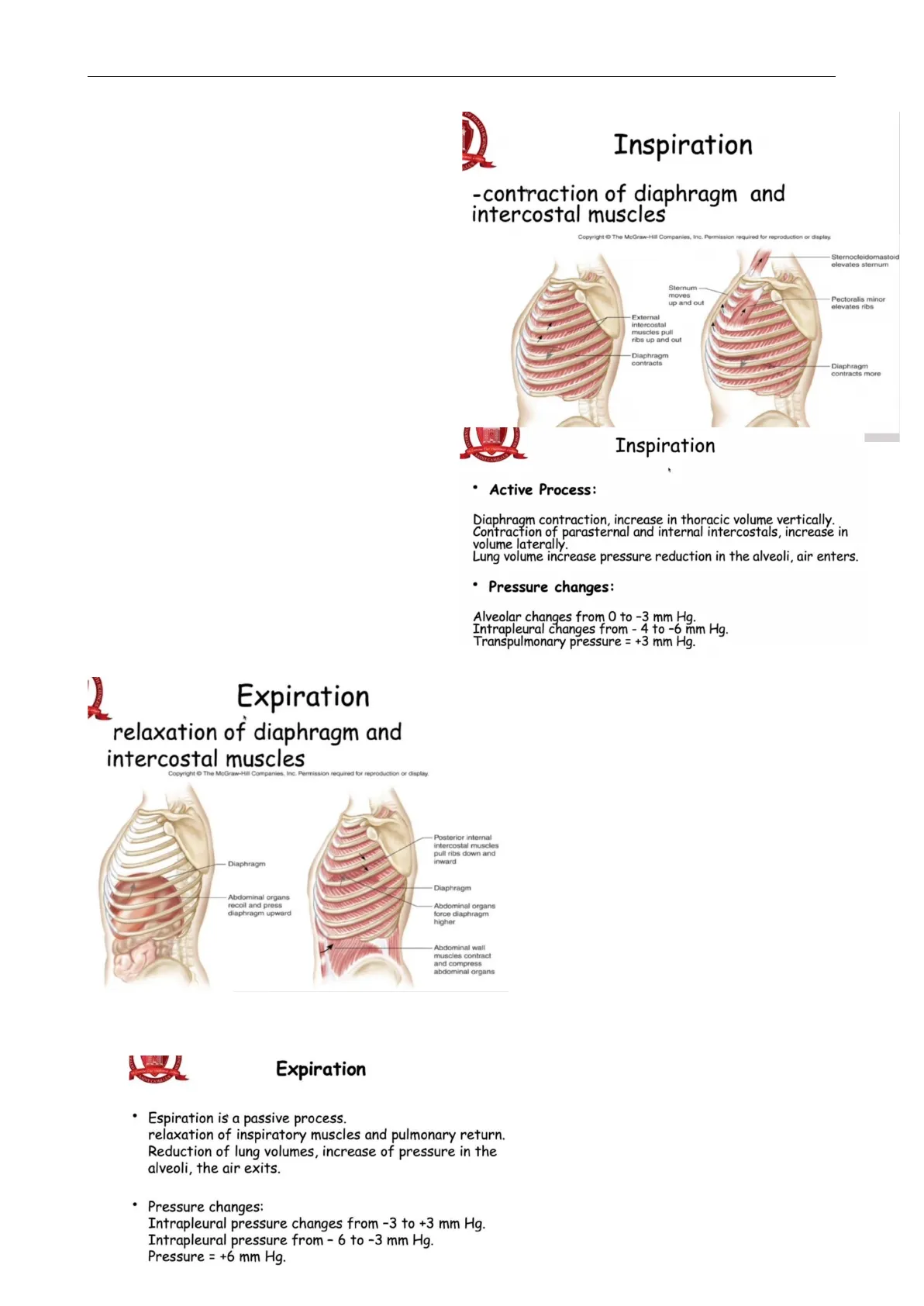
If we have some variations in this balance we can develop also a pathological condition. Remember that inspiration is an active process physiologically, it depends for 90% of the work by the contraction of the diaphragm and in assistance the intercostal muscles. Remember that external intercostal muscles are involved as auxiliary muscles in this inspiration, it is particularly important because when the subject starts to use the auxiliary muscles it may mean that the inspiration process is becoming more cost-effective for the patient. External intercostal muscles, sternocleidomastoideole, and pectoralis minor all together perform the inspiratory action. According to the active nature of inspiration, when we study the development of some diseases which determine deterioration in the inspiratory capacity we must remember that, from the physiological point of view, the inspiration remains an active process.
W HEALTH Inspiration -contraction of diaphragm and intercostal muscles Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Sternocleidomastoid elevates sternum Sternum moves up and out Pectoralis minor elevates ribs External intercostal muscles pull ribs up and out Diaphragm contracts Diaphragm contracts more NWALNI CIEN Inspiration
- Active Process: Diaphragm contraction, increase in thoracic volume vertically. Contraction of parasternal and internal intercostals, increase in volume laterally. Lung volume increase pressure reduction in the alveoli, air enters.
- Pressure changes: Alveolar changes from 0 to -3 mm Hg. Intrapleural changes from - 4 to -6 mm Hg. Transpulmonary pressure = +3 mm Hg.
Passive Expiration Process
2 Expiration relaxation of diaphragm and intercostal muscles Copyright O The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm Posterior internal intercostal muscles pull ribs down and inward Diaphragm Abdominal organs recoil and press diaphragm upward Abdominal organs force diaphragm higher Abdominal wall muscles contract and compress abdominal organs Why do we underline that? Because expiration in the physiological condition instead is a passive process, generally we don't need to spend energy to expire. In this condition when we change the nature of expiration, and expiration becomes an active process, we can find two different kinds of conditions. We are in a condition for example of sport or some voluntary expiratory act, or we are in a pathological condition in which expiration becomes more difficult and the subject may spend energy to expire. I know that Prof. Rogliani in the first lesson introduces you to asthma. Asthma is an airways obstructive disease, imagine that in presence of obstruction of the airways patient to expire need to spend energy to overcome the obstruction of the airways. Also diaphragm is involved in expiratory act, but remember internal the intercostal muscles and abdominal wall muscles are integrated to support the expiration.
Expiration
- Espiration is a passive process. relaxation of inspiratory muscles and pulmonary return. Reduction of lung volumes, increase of pressure in the alveoli, the air exits.
- Pressure changes: Intrapleural pressure changes from -3 to +3 mm Hg. Intrapleural pressure from - 6 to -3 mm Hg. Pressure = +6 mm Hg.
Respiratory System Diseases #3 - Prof. Coppola - Respiratory Physiology Page 3 of 23
Equation of Motion in Respiratory Dynamics
Understanding the Equation of Motion
1.2 Equation of motion Moreover, to understand what happens to the Presti Ptot { Pel + Pres)+ inertia respiratory system you have to take into account the so-called equation of motion. The equation of motion is just a formula that integrates the Airways (Trachea, Bronchi, Terminal Bronchioles) measured pressures which are involved in the Lungs Chest wall respiratory dynamics. First of all, we have to take into account that the system in the static NO FLOW !!!! FLOW !!! condition has a proper pressure which is due to the elements that we saw before (lung, cage, and muscles), but also we have, during the dynamic phases, a pressure which is determined by the condition of the airways, you have to imagine that air, during the respiration, moves towards airways, which is similar to tubes, so the diameter of the tubes reflects the pressure generated and the resistance generated to the movement. And then inertia, which is the coefficient that the muscles and any structure have to overcome to move.
Pleural Space and Pressure Balance
Why that? The cage and the system (a) Normal lung at rest constituted by bones, cartilaginous b 0 fissures, and muscles tend to enlarge the d 0 Ribs 0 thorax; the lungs and their elastic recoil tend to collapse. When they are in 6000 balance we are in the position of rest, you know perfectly how the lungs remain Intrapleural space attached to the cage, do you remember? Thanks to the pleural space, which is a Pleural membranes sort of vacuum which keep the lungs attached, that's why in the pleural space Diaphragm we found a negative pressure because it's a sort of a bottle of marmalade, you know, before opening you feel the air which enters, but is due to the different forces that stress the pleural space.
P = - 3 mm Hg Intrapleural pressure is subatmospheric. Elastic recoil of the chest wall ,Fiastic recoil of lung creates stem Diseases tries to pull the chest wall outward. an inward pull. 2 Pleural Pressure A Mean pleural pressure -12 cmH2O Mean pleural pressure -2.5 cmH,0 Mean pleural pressure -2 cmH2O Prof Comoa . Resaltar System INTERNATT Pleural Pressure A B Plp<Psp- Mean ple pressur -12 cml Plp=Psp Gradient of pleural liquid pressure (0.6-1.0 cmH2O) -2 cmH30 Gradient of pleural surface pressure (0.1-0.4 cmH2O) - 1 cmH20 0 cmH2O + 1 cmH20 Mean pleural pressure 2 cmH,O Plp>Psp + 2 cmH30 + 3 cmH2O + 4 cmH20 Prof. Coppola - Respiratory System DiseasesRespiratory System Diseases #3 - Prof. Coppola - Respiratory Physiology Page 4 of 23
Pneumothorax and Pleural Effusion
That's why if we produce damage in the cage, and we create a communication between the pleural space and the external environment, I can enter in the pleural space, the lung collapses and the cage enlarges, in this condition, the pressure in the pleural space is no more negative and becomes of course in balance with the external pressure. The same happens in the condition of pleural effusion in which we have no air in the pleural space, but we have an increase of liquid and in these cases, the pressure remains negative.
Pleural Pressure Pneumothorax Chest wall Pleural sac Air Palv = 0 mm Hg Lung Palv = 0 mm Hg Pip = - 4 mm Hg- Pip = 0 mm Hg- (a) (b) Chest wall Lung TLC 100 75 volume FRC Respiratory system 50 25 RV Neg (-) 0 Pos (+) Prof Pressure (cm H,O) my System Diseases And this is what happens in a condition which is called pneumothorax when the negative pressure of the pleural space became in balance with the external pressure and we assist to a collapse of the lung, and of course, the ability of the lung to remain attached to the thorax fail, and no ventilation can be produced in this kind of condition.
Work of Breathing
This diagram is just to keep in mind that the work of breath, which is the expenditure of energy that we need to produce ventilation can vary considerably according to the modification of the chest wall and lung balance.
Compliance and Elastance in Lung Function
Understanding Compliance and Elastance
1.3 Compliance and elastance ASITY OF MONTH SCIE Compliance/Elastance CAMEL Pulmonary compliance (or lung compliance) is a measure of the lung's ability to stretch and expand. · Static lung compliance is the change in volume for any given applied pressure. . Dynamic lung compliance is the compliance of the lung at any given time during actual movement of air. Elastance, also known as the elastic resistance is the reciprocal of compliance, i.e. the pressure change that is required to elicit a unit volume change. This is a measure of the resistance of a system to expand. And this is another concept that you must know and underline: the concept of elastance and compliance. This concept in pathology is determinant (alterations of compliance and elastance). Compliance is a measure of the lung's ability to stretch and expand when receiving pressure. Elastance is the opposite and represents the resistance of the lung to modify its volume when it receives pressure.
Image the lung as a balloon, we have different kinds of a balloon, if we have a balloon with high compliance it means that is enough very small effort to enlarge the balloon, if we have a balloon with very low compliance we need a greater effort to enlarge the balloon. The opposite is for the elastance. So if we have a balloon with high elestance, we need a greater effort; low elastance, low 4