Upper Airways Pathology: Carcinoma, Polyps, and Vasculitis
Document from University about Upper Airways. The Pdf, suitable for university students of Biology, covers the pathology of the upper airways, including squamous cell carcinoma of the oral cavity and larynx, nasal polyps, fungal infections like aspergillosis, and autoimmune vasculitis.
See more11 Pages
Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Upper Airways Pathology
18.10.2023
Prof. Ponzoni
Author: Selin Satar
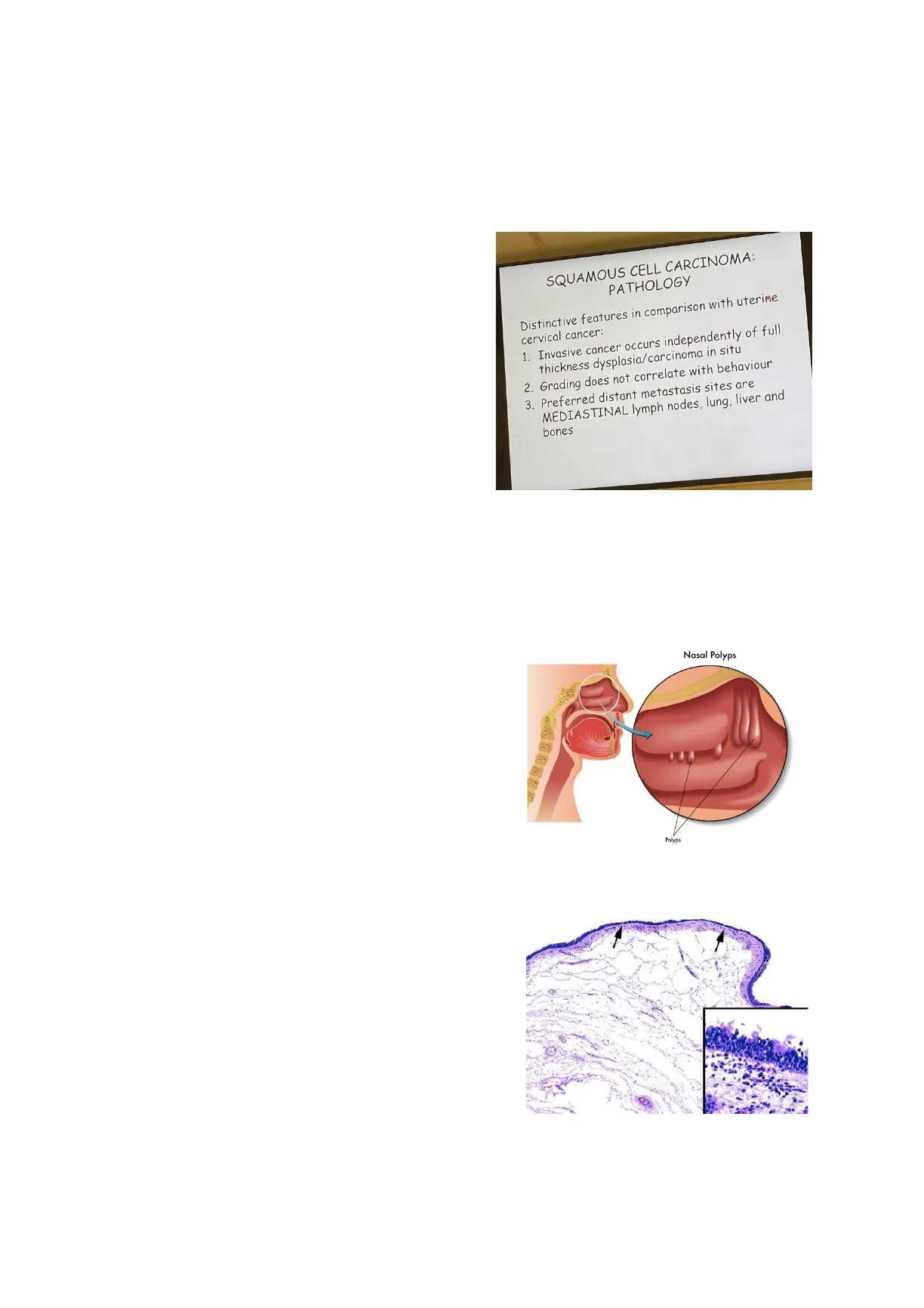
Squamous Cell Carcinoma Recap
Recap of the last lesson:
We analysed squamous cell carcinoma of the
oral cavity. The slide below summarizes what we
discussed and remember that the squamous cell
SQUAMOUS CELL CARCINOMA:
PATHOLOGY
carcinoma of the oral cavity and the cervix are
the famous ones. We discussed the similarities
Distinctive features in comparison with uterine
cervical cancer:
and the differences between these two types of
1. Invasive cancer occurs independently of full
thickness dysplasia/carcinoma in situ
cancers. Remember that oral cavity squamous
cell carcinoma may present metastasis to the
2. Grading does not correlate with behaviour
3. Preferred distant metastasis sites are
MEDIASTINAL lymph nodes, lung, liver and
bones
mediastinal lymph nodes. How do you stage the
cancer in the oral cavity? With PET scan if you
are rich, if you are not rich you order CT scan
from skull to the feet. (Professor quoted like
this). We also must look at the chest and mediastinal lymph nodes together with the
abdomen. Mediastinum is the place contained between lungs and the hearts. Lungs and the
heart border the mediastinum. Upper airways, thoracic cavity and thymus are inside the
mediastinum. Thymus is prominent in children, and it becomes smaller as a person ages.
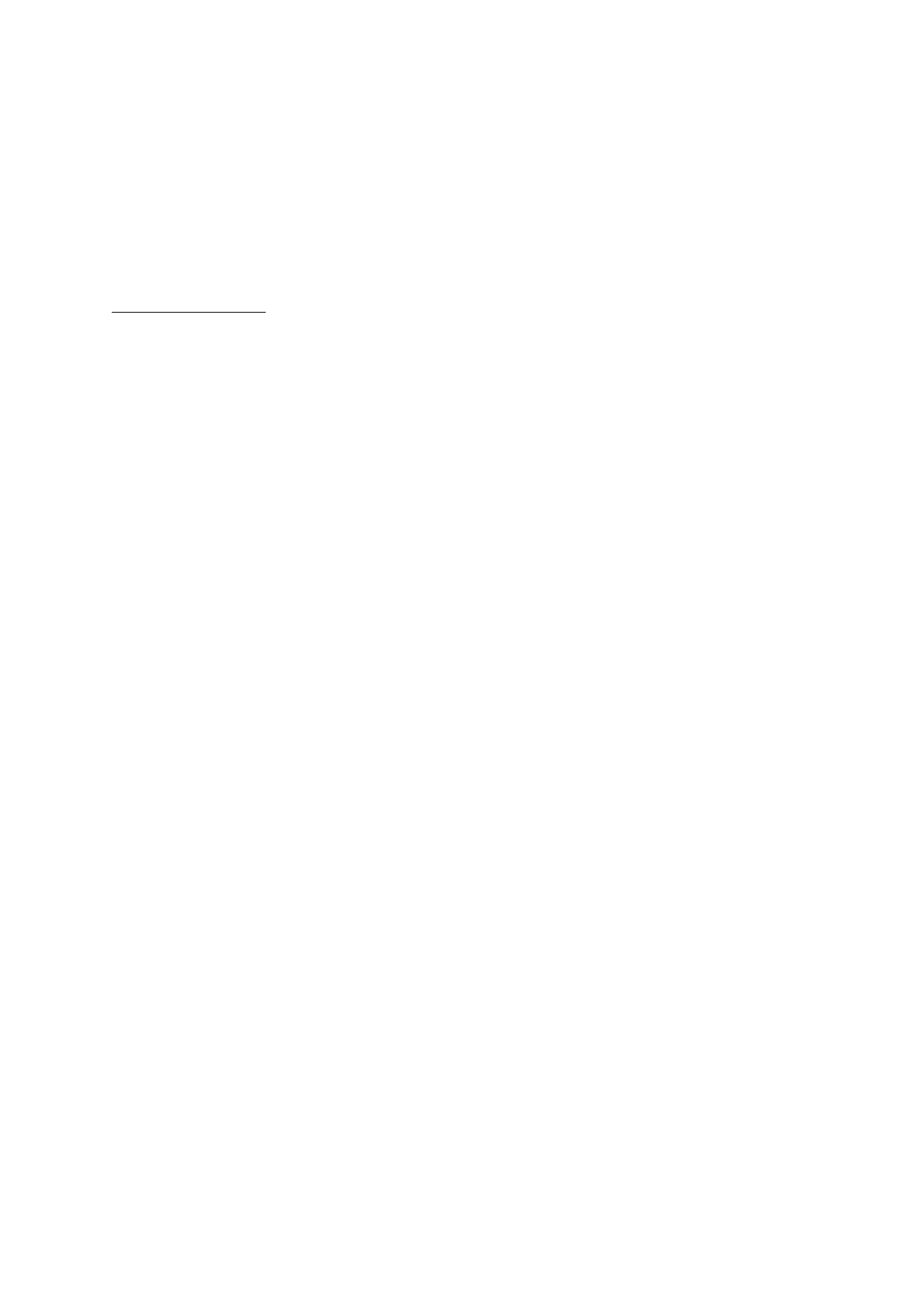
Nasal Polyps
Another anatomical site that we must cover in the
Nasal Polyps
head and neck region are upper airways. Upper
airways are usually related to the nasal cavity. In
the nasal cavity we have a very common disorder
which are nasal polyps. They are polypoidal<
formations that are covered by a normal
respiratory tract epithelium (ciliated
pseudostratified epithelium). In the picture we can
see the polypoidal appearance that is given by an
Polyps
increase of mucopolysaccharides in the stroma. There are few cells, but vast majority of the
tissue is plumped and there are plenty of mucopolysaccharides which give expansion to the
mucosa. They are totally benign lesions, they are not tumors or neoplastic lesions.
Sometimes these lesions occur in a particular
population who are allergic. Allergic people suffer
from rhinitis.
If rhinitis is chronic eventually the person can
develop this polypoidal appearance. In fact, in the
stroma, you can find few inflammatory cells which
are eosinophils.
1Author: Selin Satar
Prof. Ponzoni
18.10.2023
Fungal Infections in Upper Airways
Upper airways are target of some infections as well. One of the most common infections in
this area are fungi in particular Mucor. We have two fungi which are related to nasal sinuses:
Aspergillus Fumigatus and Mucor. We can have some abscesses which are encapsulated
inflamed lesions which can be caused by fungi. Fungi can survive because we are
immunocompetent but in patients who are immunodeficient, fungi are very prominent and
can cause serious problems.
Professor's question: Can you provide me a situation in which you can have such
superimposed fungal infection?
Immunosuppression and Fungal Infection
In patients who had transplantation there can be superimposed fungal infection. According to
the organ that the patient received, the immunosuppression differs. For example, a patient
undergoing a heart transplant receives much more immunosuppressive therapy compared to
a patient who received a kidney. Also don't forget the bone marrow transplantation. In my
personal experience when we started to study bone marrow transplantation, I remember a
group of patients was receiving bone marrow transplantation. They were transferred from
another hospital where their clinical condition worsened so they preferred to avoid
transplanting these patients and let them die. As the last choice they came to our hospital,
and I remember that I found several times mostly in the lungs but also in the airways some
fungal abscesses which are caused by aspergillus fumigatus. We couldn't figure out why
aspergillus caused it. The reason that we discovered this was there were plenty of
aspergillus fumigatus in the hospital. For healthy people contact with aspergillus is not a
dramatic issue but if you are deeply immunosuppressed it plays a difference. That's why I
don't see anybody that dies from aspergillus infection in a few exceptions. There is another
situation that is at risk, and it is much more common. It's created with the air conditioner.
You must check the status of your air conditioner in your car because there can be some
fungi. Another situation in which you have a significant pathological change in the airways is
due to some autoimmune disorders. Our body becomes antigenic to some antibodies since
you got an autoreactive system. Sometimes there is a situation in which this interaction
occurs around the vessels which is called vasculitides. Vasculitides is an autoimmune
manifestation.
Vasculitides in Upper Airways
Lymphocytes infiltrate around the vessels and these lymphocytes may destroy these vessels
because they are not recognized anymore as cells. One of the most frequent situations of
vasculitides in the upper airways is provided by granulomatosis with polyangiitis (this is the
name of the disease). The former term of this disease is Wegener disease which is not used
anymore. We expect to see vessels that are infiltrated by granulomata. Granulomata is a
collection of macrophages. We have a granuloma with perivascular infiltration of
lymphocytes. This infiltration also involves the wall of the small arteries which destroys them.
When we destroy the arterial wall of the small vessel the tissue becomes ischemic. If we
stop the blood flow the cell dies. Summing up in this situation there is a collection of inflamed
vessels with tissue necrosis. There is a situation in the nasal cavity that is not related to the
vasculitis of the nasal cavity but is very important to keep in mind. The basis is somewhat
the same but potent enough you can solve the problem in another way because if you treat a
patient with vasculitis you have to use so many corticosteroids and the prognosis is not so
good.
2Author: Selin Satar
Prof. Ponzoni
18.10.2023
Necrosis and Vasculitis in Nasal Cavity
There is another situation where you have necrosis with a vasculitis and some inflammatory
cells in the nasal cavity. This is a real story that happened to us our department received
three cases in one week with a morphology of granulomatosis with polyangiitis. This disease
is very rare, so we didn't understand how we received three cases in a week. One of us
called the clinician and the clinician told us that the patient didn't have regular
granulomatosis. There is a mechanism that can narrow the vessels in the nasal cavity
(vasoconstriction). So, the technical term for the nose bleeding is called epistaxis. Some
people can experience epistaxis for several reasons. People can take drugs such as nasal
sprays that contain catecholamines which can constrict the vessels, or they can obtain
vasoconstriction because of cocaine abuse. Both conditions can cause epistaxis. All three
patients that had granulomatosis were cocaine users. The important thing to notice before
diagnosing a patient with granulomatosis is knowing whether the patient uses cocaine or not.
Cocaine abuse is a psychiatric condition, and it is not treated with corticosteroids which are
used in granulomatosis.
Neoplastic Disorders of Upper Airways
Another situation that we can have in the upper airways are neoplastic disorders. One of
them is lymphoma which we will cover in the second semester in haematology. Lymphoma
may arise from B cells or K cells. Some lymphomas that arise from B or K cells are
associated with upper airways.
Another disease that may arise in the upper airways are caused by tumors. There are many
tumors.
- Sinonasal papilloma
- Olfactory neuroblastoma (esthesioneuroblastoma)
- NUT midline carcinoma
- Nasopharyngeal carcinoma
Sinonasal Papilloma
Sinonasal Papilloma
Papilloma means a tumor with a
papillary appearance. It is usually
benign. The malignant counterpart is
called papillary carcinoma. This
sinonasal papilloma has two ways of
growing. The papilloma can develop
in such a way that can be exophytic
(grows externally in the nasal cavity) but sometimes the growth of this papilloma occurs
internally which makes the inverted papilloma (grows within the wall of the nasal cavity).
They are biologically benign tumors but they can cause some problems. The rate of
recurrence is higher in inverted papilloma. During surgery the surgeon sends us a potential
inverted papilloma to ensure that the resection margins are free of disease. This papilloma is
HPV-associated (HPV 6 and HPV 11). They need to be removed because they can grow
and growing may compress some important structures such as nerves. About 1 out of 10
cases can transform into malignant tumor if they are not removed.
a
Inverted Papilloma, Case 2
b
Exophytic Papilloma, Case 4
318.10.2023
Prof. Ponzoni
Author: Selin Satar
Olfactory Neuroblastoma
Olfactory neuroblastoma (esthesioneuroblastoma)
When we analyse the mucosa of the upper limit of the
nasal cavity there are some cells with dual potential
differentiation in terms of epithelial and neural. They
are called neuroectodermal olfactory cells. This tumor
arises because of neoplastic transformation of
neuroectodermal olfactory cells. There are two peaks
of incidence one in teenagers (15 years) and one in
middle aged people (50 years). Survival rate differs
amongst patients which got their tumor removed and
received chemotherapy. The rate is between 40-90%.
The broad range may be due to the early diagnosis. In the picture you
can see the clinical manifestation of the olfactory neuroblastoma. There
are some nests and lobules in these tumors with undifferentiated
appearance (they are rounder). In our body undifferentiated many cells
are round too. This way of arrangement is also characteristic because
these nests are separated by fibrovascular stroma so bends of collagen.
Identifying these cells is not always possible with morphology. We have to use
immunohistochemistry and find some markers which can find cells with neuroendocrine
origin. Some markers that fulfill this task are neuron-specific- enolase, synaptophysin, CD56
and chromogranin. To ensure that these cells have neuroendocrine phenotype they should
express these markers. So, if you want to confirm the nature of these tumors you cut
additional slides and stain them individually with neuro-specific enolase, CD56 and so on. In
the picture below we can see nests of cells and a pinkish material that are bent. These are
fibrovascular cores.
NUT Midline Carcinoma
Nut Midline Carcinoma
Another tumor that we have in this area is
called nut midline carcinoma. It is called
midline because it involves not only head and
neck region, but it involves some structures
along the midline such as salivary glands,
nasopharynx, of thorax and abdomen. This
tumor has no age preference. In comparison
with the previous one this one is very
aggressive. In our decade to have a disease
with less than one year of life expectancy
means that this is a very aggressive tumor. So how can we suspect this tumor? This is what
we see under the microscope. They look like squamous cells. They are large cells and have
a pink cytoplasm. Nut midline carcinoma has a dual component made by squamous cells
and undifferentiated cells. This component is responsible for the aggressiveness of the
tumor. We have to see both components to diagnose the disease.
4