Pulmonary Circulation and Gas Diffusion, UAG School of Medicine Presentation
Slides from Uag School of Medicine about Pulmonary Circulation. The Pdf provides a detailed overview of pulmonary circulation and gas diffusion, including learning objectives, principles, pulmonary zones, edema development, and Fick's law. This University level Biology material is designed for medical students.
See more40 Pages

Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Pulmonary Circulation Overview
Pulmonary Circulation
Dra. Carla Romo
Anesthesiology / Critical Care
2025-1
UAG
SCHOOL OF MEDICINE
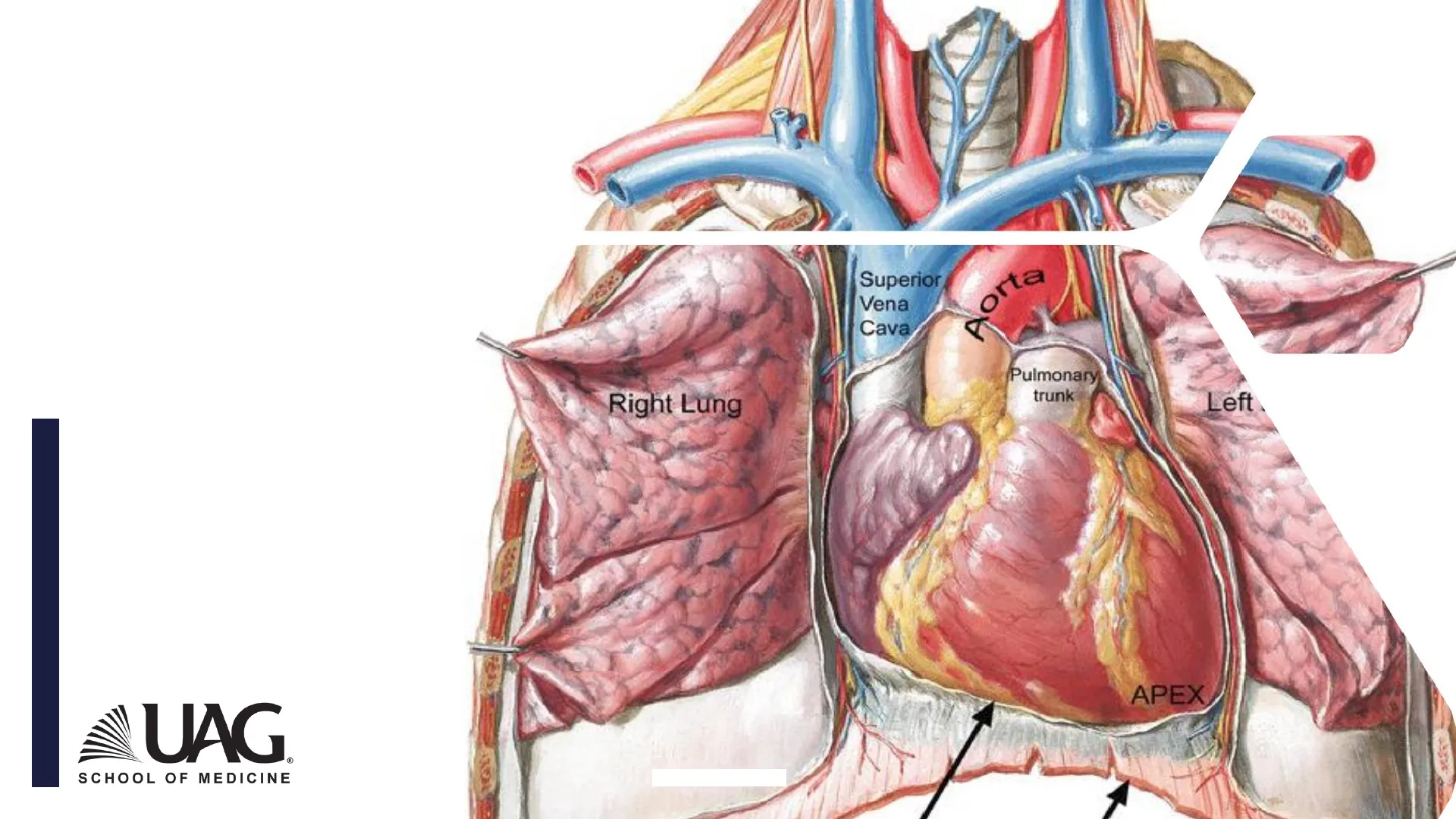
Right Lung
Superior
Vena
Cava
orta
Pulmonary
trunk
Left
APEX
- Contrast systemic and pulmonary circulations in terms of pressures, resistance to blood flow,
and response to hypoxia. - Recall Ohm's law and apply it to understand pulmonary circulation.
- Complement Fick's principle by calculating the content of oxygen.
- Describe the roles of distention and recruitment of pulmonary vessels in altering pulmonary
blood flow and pulmonary vascular resistance. - Define zones I, II, and III in the lung with respect to pulmonary vascular pressure and alveolar
pressure. - Explain how alveolar pressure, blood flow, and gravity interact to influence the function of each
zone. - Describe the consequence of hypoxic pulmonary vasoconstriction on the distribution of
pulmonary blood flow. - Explain the development of pulmonary edema through:
- Increased hydrostatic pressure
- Increased permeability
- Impaired lymphatic outflow or increased central venous pressure.
UAG
SCHOOL OF MEDICINE
OBJECTIVES
Pulmonary and Systemic Pressures
Mean = 15
Mean = 100
25
120
8
80
Artery
= 12
Pulmonary
Systemic
25
0
120
0
RV
LV
Cap
Cap
20
RA
LA
2
5
=8
10
Vein
Vein
UAG
SCHOOL OF MEDICINE
West. Respiratory Physiology.2013.
Artery
30
Pulmonary Circulation Characteristics
PULMONARY CIRCULATION
LOW - RESISTANCE
NETWORK
HIGH - DISTENSIBLE
VESSELS
PULMONARY BLOOD
FLOW = 100% OF CO
LOW PRESSURE
SYSTEM
UAG.
SCHOOL OF MEDICINE
Mean Pressures in Circulation
MEAN PRESSURES
- Pulmonary artery
15
mmHg - Aortic pressure
100
mmHg - Right atrium
2
mmHg - Left atrium
5
mmHg - Right ventricle
25
mmHg - Left ventricle
120
mmHg
Interventricular
Apex
Septum
Mitral Valve
LV
RV
Tricuspid
Valve
RA
LA
Interatrial
Septum
UAG.
SCHOOL OF MEDICINE
Ohm's Law and Pulmonary Vascular Resistance
What states Ohm's law and how can we use it to
calculate the Pulmonary vascular resistances?
Q = AP/R
UAG
SCHOOL OF MEDICINE
Calculating Pulmonary Vascular Resistance (PVR)
PULMONARY VASCULAR RESISTANCE (VR)
R =4P
Q
R = input pressure (Pi) - output pressure (Po)
Blood flow
PVR = (15 - 5)
6
PVR = 1.7 mmHg / L / min
UAG
SCHOOL OF MEDICINE
Pi = 15 mmHg (MAP)
Po = 5 mmHg (LAP)
BF = 6 L / min ( CO)
Pulmonary Artery Characteristics
Pulmonary artery CHARACTERISTICS
IS SHORTER THAN
AORTA
WALLS ARE THINNER
THAN AORTA
WALLS HAVE LESS
SMOOTH MUSCLE
PULMONARY VEINS
ARE THINNER
UAG
SCHOOL OF MEDICINE
Alveolar Vessels and Transmural Pressure
ALVEOLAR VESSELS
- Transmural pressure: pressure difference between
the inside and outside of vessels. - Alveolar vessels:
- Depend on the alveolar pressure.
- When alveolar pressure rises above the capillary
pressure > capillary will collapse.
-
UAG.
SCHOOL OF MEDICINE
Alveolar Vessels Resistance
ALVEOLAR VESSELS
Alveolus
Alveolar vessels
Resistance
Extra-alveolar
vessels
A
A
_
Lung volume
+
West. Respiratory Physiology.2013.
UAG
SCHOOL OF MEDICINE
Extra-Alveolar Vessels
EXTRA-ALVEOLAR VESSELS
- Arteries
- Veins
Their caliber is affected by lung volume
As the lung expands > caliber increase
UAG
SCHOOL OF MEDICINE
Resistance
_
Lung volume
+
West. Respiratory Physiology.2013.
Total Pulmonary Vascular Resistance
A
B
C
Resistance
_
Lung volume
West. Respiratory Physiology.2013.
+
Alveolar vessels
resistance
B
A
Extraalveolar vessels
resistance
UAG.
SCHOOL OF MEDICINE
C
Total pulmonary vascular resistance
Vascular Recruitment and Distension
What is the difference between vascular
recruitment and distention?
Recruitment
Distension
-
UAG.
SCHOOL OF MEDICINE
West. Respiratory Physiology.2013.
Pulmonary Blood Flow and Fick's Principle
PULMONARY BLOOD FLOW
- Fick's principle
Q: Volume of blood passing throw the lungs each minute
VO2: O2 consumed per minute
CaO2: Oxigen concentration in the blood leaving the lungs
CV02: Oxigen concentration in the blood entering the lungs
VO2 = Q (Ca02 - CV02)
Q =
VO2
_
(Ca02-CvO2)
Arteriovenus oxygen difference
UAG
SCHOOL OF MEDICINE
Oxygen Content Calculation
Oxygen content
Sum of oxygen bound to hemoglobin and
dissolved in plasma within arterial blood
- Ca02 = [1.34 x Hb x (SaO2/100)] + (0.003x PaO2)
Arterial oxygen content is directly
proportional to the Hb, SaO2, and PaO2 - Hb (g/dL) = hemoglobin
concentration - SaO2 (%) = arterial oxygen
saturation in hemoglobin - PaO2 (mm Hg) = partial pressure of
oxygen - 1.34 (mL) = maximum oxygen binding
capacity of 1 g of hemoglobin. - 0.003 = solubility coefficient of
oxygen in plasma
UAG.
SCHOOL OF MEDICINE
18
Distribution of Blood Flow in the Lung
DISTRIBUTION OF BLOOD FLOW
- Blood flow decreases
from bottom to the top - Bottom -> resistance v
(more recruitment or
distention).
UAG
SCHOOL OF MEDICINE
150
Radiation
counters
Blood flow/unit volume
100
50
Bottom
Top
0
0
5
10
15
20
25
Distance up lung (cm)
West. Respiratory Physiology.2008.
West Zones of the Lung
Zone 1
PA>Pa>Pv
Pa= pressure
in the artery
PA= pressure
in the alveoli
Alveolar
Zone 2
Pa>PA>Pv
PA
Pv= pressure
in the vein
Pa
1
Pv
1
Arterial
Venous
Distance
E
Zone 3
Pa>Pv>PA
Blood flow
-
UAG
SCHOOL OF MEDICINE
West. Respiratory Physiology.2008.
WEST ZONES
Active Control of Circulation
ACTIVE CONTROL OF CIRCULATION
100
I
1
1
80
60
40
20
0
50
100
150
200
300
500
ALVEOLAR PO2
- Changes in alveolar PO2
- "Hypoxic pulmonary vasoconstriction"
UAG.
SCHOOL OF MEDICINE
West. Respiratory Physiology.2008.
BLOOD FLOW (% CONTROL)
Hypoxic Pulmonary Vasoconstriction
HYPOXIC
PULMONARY
VASOCONSTRICTION
UAG
SCHOOL OF MEDICINE
- Is independent of CNS.
- Some chemical mediators interacting in
this process: - Catecholamines.
- Histamine.
- Angiotensin.
- Prostaglandins.
- Decrease in vasodilators as Nitric
oxide (Fetal life).
O2 = 150 mm Hg
CO2 = 0 mm Hg
O2 = 100 mm Hg
CO2 = 40 mm Hg
O2 = 40 mm Hg
CO2 = 45 mm Hg
O2 = 100 mm Hg
CO2 = 40 mm Hg
O2 = 150 mm Hg
CO2 = 0 mm Hg
Decreased O2
Increased CO2
02 = 40 mm Hg
CO2 = 45 mm Hg
Decreased O2
Increased CO,
A
The reflex
constriction of the
vessel is the
response to the
alveolar hypoxia
O2 = 150 mm Hg
CO2 - 0 mm Hg
Decreased O2
Increased CO2
O2 - 40 mm Hg
CO2 = 45 mm Hg
Decreased O2
Increased CO2
UAG
@
C
SCHOOL OF MEDICINE
B
O2 = 100 mm Hg
CO2 = 40 mm Hg
Decreased O,
Increased CO2
Î
The PO2 is still low,
but less amount of
blood is going
through this unit
D
Water Balance in the Lung
WATER BALANCE IN THE
LUNG
- Only 0.3 micrometers of tissue separates
the capillary blood from the air in the lung - Fluid exchange across the capillaries
walls is believed to obey "Starling's Law"
UAG
SCHOOL OF MEDICINE
(h) Exchange surface of alveoli
Alveolar
epithelium
Nucleus
endothelia
Capillary
Endothelium
0.1-
1.5
um
Surfactant
Fused basement
membranes
Alveolar air space
Silverthorn. Human Physiology.2001
Capillary Pressure Values
VALUES
Capillary Colloid osmotic
pressure:
28 mmHg.
Capillary hydrostatic pressure:
Higher at bottom of the lung than at the
top.
Colloid osmotic pressure on
interstitial fluid
20 mmHg in lung lymph.
UAG
SCHOOL OF MEDICINE
Pulmonary Edema Development
EDEMA
- Early stage of edema. Interstitial
edema. Engorgement of
perivascular and peribronchial
spaces. - Later stages -> Water crosses the
alveolar epithelium into the
alveolar space. Unventilated and
no gas exchange.
Alveoli
Alveolar space
2
Interstitium
Capillary
Alveolar wall
1
Bronchus
O
Artery
/
Perivascular space
UAG
SCHOOL OF MEDICINE
West. Respiratory Physiology. 2008
Diffusion of Gases
DIFFUSION OF GASES
UAG
SCHOOL OF MEDICINE
Diffusion Objectives
Objectives
- State the Fick's law for diffusion and determine the limitations of gas transfer.
- Define oxygen diffusing capacity and describe the use of carbon monoxide to
determine oxygen diffusion capacity. - Name the factors that affect diffusive transfer of gas.
UAG
SCHOOL OF MEDICINE
Characteristics of Gas Transfer
CHARACTERISTICS
PA
C
A
A
A
UAG
SCHOOL OF MEDICINE
- Area of blood-gas barrier in the
lung: 50 to 100 m2. - Thickness: only 0.3 m in many
places. - The rate of transfer is
proportional to a diffusion
constant, which depends on
the properties of the tissue and
the particular gas.
12
CO2
Transfer of gases
through cellular
membranes or
capillary walls
functions through
"SIMPLE
DIFUSSION"
UAG
SCHOOL OF MEDICINE
Fick's Law and Gas Transfer Limitations
WHAT STATES FICK'S LAW REGARDING GAS EXCHANGE
AND WHAT FACTORS LIMIT GAS TRANSFER?
PAO2 = 100
PACO2 = 40
CO2 O2
PvO2 40
PvCO2 45
I
I
0
time/sec
0.75
100
I
PaO2
-
UAG
®
40
SCHOOL OF MEDICINE
Start of
capillary
End of
capillary
Alveolar
N2O
O2 (Normal)
O2 (Abnormal)
Partial pressure
CO
0
0.25
0.50
0.75
Time in capillary (s)
UAG
SCHOOL OF MEDICINE
Picture from Respiratory Physiology, West
Diffusion vs. Perfusion Limited Gas Transfer
DIFFUSION VS PERFUSION LIMITED
Diffusion limited
- E.G. Carbon monoxide (CO)
" CO strong bonds with Hb
" Increases in CO content result in very
minimal increase in partial pressure
Partial pressure difference still exists (when
blood finishes its passage through the alveoli)
Transfer of CO is limited by the rate of
diffusion, not the amount of blood available
02 in certain conditions (emphysema,
fibrosis, intense exercise)
Perfusion limited - E.G. Nitrous oxide (N20)
. N20 doesn't form bond with Hb
. Increase in N20 content result in rapid rise
in partial pressure
· Equilibrium is reached very early on
. Transfer of N20 is limited by the amount of
blood available
. 02 in normal conditions is perfusion limited
· CO2 is perfusion limited
UAG.
SCHOOL OF MEDICINE
UAG
SCHOOL OF MEDICINE
A
Mild affection of O2
and CO2 exchange
B
Severe affection Alveoli
completely filled
105
Normal
B
PaO2
exercise
I
40
0
time
.75B
Alveolar
50
I
Normal
I
I
Abnormal
Po2 mm Hg
Î
Grossly abnormal
Exercise
0
0
0.25
0.50
0.75
Time in capillary (s)
UAG
SCHOOL OF MEDICINE
Picture from Respiratory Physiology, West
UAG.
SCHOOL OF MEDICINE
Pco2 mmHg
45
I
ABNORMAL
I
NORMAL
I
1
40
+
ALVEOLAR
I
EXERCISE
1
0
.25
.5
.75
Time in Capillary - sec
Picture from Respiratory Physiology, West
Diffusing Capacity of the Lung
DIFFUSING CAPACITY
Vgas . A.D. P -P2 )
T
Vgas = DL . (P1 - P2)
DL = Diffusing capacity of the lung
- Rate at which the gas is diffused through the alveolar capillary
membrane (ml/min) - Includes area, thickness and diffusion properties
UAG
®
SCHOOL OF MEDICINE
Measurement of Diffusing Capacity
MEASUREMENT OF DIFFUSING CAPACITY
Carbon Monoxide is used because is diffusion limited
Vgas = DL . (P1 - P2)
VCO
DL =
P1 -P2
Example : Carbon monoxide
P1 is partial pressure at alveolar gas
P2 is partial pressure at capillary blood
Partial pressure of CO in capillary blood is virtually zero (at non-lethal PAco)
UAG
SCHOOL OF MEDICINE
DL =
VCO
PACO
Conditions Decreasing Diffusion Capacity
What conditions decrease the diffusion capacity?
- Thickening of barrier
- Edema
- Fibrosis (sarcoidosis, scleroderma)
- Decreased uptake by red cells
- Anemia
- Reduced surface area
- Emphysema
- Tumors
- Low Cardiac Output, embolus
- Uneven VA - Q
- Reduced uptake by red cells
UAG
SCHOOL OF MEDICINE
A
CO
B
CO
C
CO
Alveolar
fibrosis
Alveolus
Capillary
Exudate
D
CO
E
CO
F
CO
- Loss of
alveoli
Alveolar
fibrosis
Pulmonary
embolus
Edema
No
blood flow
Copyright 2009 by Saunders, an imprint of Elsevier Inc.