Nutrizione e cancro: impatto degli stili di vita e dieta chetogenica
Slide dall'Università San Raffaele su Nutrizione e cancro. Il Pdf esplora la relazione tra nutrizione e cancro, l'impatto degli stili di vita e l'effetto Warburg, con dati epidemiologici e ricerche sulla dieta chetogenica e la soppressione del cancro colorettale, utile per studenti universitari di Biologia.
See more46 Pages

Unlock the full PDF for free
Sign up to get full access to the document and start transforming it with AI.
Preview
Università San Raffaele Roma
Docente Massimiliano Caprio
Nutrizione e cancroU Università San Raffaele Roma Massimiliano Caprio
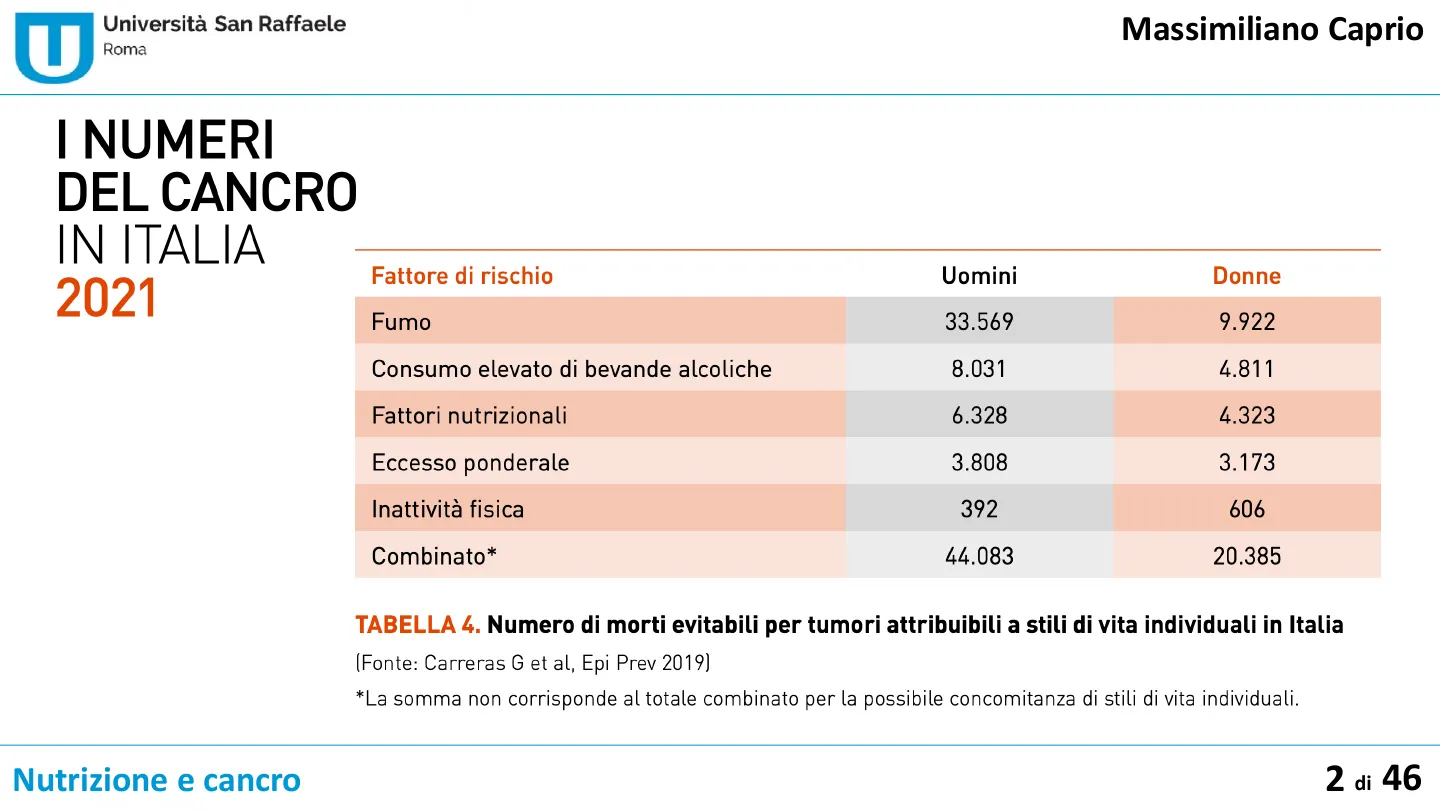
I NUMERI DEL CANCRO IN ITALIA 2021
Fattore di rischio Uomini Donne Fumo 33.569 9.922 Consumo elevato di bevande alcoliche 8.031 4.811 Fattori nutrizionali 6.328 4.323 Eccesso ponderale 3.808 3.173 Inattività fisica 392 606 Combinato* 44.083 20.385
TABELLA 4. Numero di morti evitabili per tumori attribuibili a stili di vita individuali in Italia (Fonte: Carreras G et al, Epi Prev 2019) *La somma non corrisponde al totale combinato per la possibile concomitanza di stili di vita individuali.
Nutrizione e cancro 2 di 46U
Codice Europeo Contro il Cancro
Le 12 principali modalità per ridurre il rischio di sviluppare un tumore
Università San Raffaele Roma Massimiliano Caprio Le 12 principali modalità per ridurre il rischio di sviluppare un tumore sono riassunte, a cura della Organizzazione Mondiale della Sanità, della IARC e della Commissione Europea, nel Codice Europeo Contro il Cancro
- Non fumare. Non consumare nessuna forma di tabacco.
- Rendi la tua casa libera dal fumo. Sostieni le politiche che promuovono un ambiente libero dal fumo sul tuo posto di lavoro.
- Attivati per mantenere un peso sano.
- Svolgi attività fisica ogni giorno. Limita il tempo che trascorri seduto.
- Segui una dieta sana:
- Consuma molti e vari cereali integrali, legumi, frutta e verdura.
- Limita i cibi ad elevato contenuto calorico (alimenti ricchi di zuccheri o grassi) ed evita le bevande zuccherate.
- Evita le carni conservate; limita il consumo di carni rosse e di alimenti ad elevato contenuto di sale.
- Se bevi alcolici di qualsiasi tipo, limitane il consumo. Per prevenire il cancro è meglio evitare di bere alcolici.
- Evita un'eccessiva esposizione al sole, soprattutto per i bambini. Usa protezioni solari. Non usare lettini abbronzanti.
- Osserva scrupolosamente le istruzioni in materia di salute e sicurezza sul posto di lavoro per proteggerti dall'esposizione ad agenti cancerogeni noti.
- Accerta di non essere esposto a concentrazioni naturalmente elevate di radon presenti in casa. Fai in modo di ridurre i livelli elevati di radon.
Nutrizione e cancro 3 di 46U
Sovrappeso e Obesità come Fattori di Rischio Oncologico
Stime e Impatto Globale
Università San Raffaele Roma Massimiliano Caprio · Sovrappeso e obesità sono importanti fattori di rischio oncologico · Secondo stime del World Cancer Research Fund, il 20-25% dei casi di tumore sarebbe attribuibile a un alterato bilancio energetico, legato al binomio eccesso ponderale e sedentarietà · Secondo le stime dell'Institute for Health Metrics and Evaluation all'eccesso ponderale sarebbero attribuibili 5 milioni di decessi in tutto il mondo nel 2019 (pari al 9% di tutti i decessi) e complessivamente oltre 40 milioni di anni vissuti con disabilità.
Nutrizione e cancro 4 di 46U
Body Fatness and Cancer - Viewpoint of the IARC Working Group
Revisione sistematica e tumori associati all'eccesso ponderale
Università San Raffaele Roma Massimiliano Caprio The NEW ENGLAND JOURNAL of MEDICINE SPECIAL REPORT Body Fatness and Cancer - Viewpoint of the IARC Working Group Beatrice Lauby-Secretan, Ph.D., Chiara Scoccianti, Ph.D., Dana Loomis, Ph.D., Yann Grosse, Ph.D., Franca Bianchini, Ph.D., and Kurt Straif, M.P.H., M.D., Ph.D., for the International Agency for Research on Cancer Handbook Working Group Revisione sistematica di oltre 1000 studi sulla relazione tra peso corporeo e rischio di cancro Identificati 13 tumori per i quali esiste chiara associazione con l'eccesso ponderale
Nutrizione e cancro 5 di 46U
Strength of the Evidence for a Cancer-Preventive Effect of the Absence of Excess Body Fatness
Associazione tra peso corporeo e rischio di cancro
Università San Raffaele Roma Massimiliano Caprio Table 2. Strength of the Evidence for a Cancer-Preventive Effect of the Absence of Excess Body Fatness, According to Cancer Site or Type." Cancer Site or Type Strength of the Evidence in Humans? Relative Risk of the Highest BMI Category Evaluated versus Normal BMI (95% CI)# Esophagus: adenocarcinoma Sufficient 4.8 (3.0-7.7) Gastric cardia Sufficient 1.8 (1.3-2.5) Colon and rectum Sufficient 1.3 (1.3-1.4) Liver Sufficient 1.8 (1.6-2.1) Gallbladder Sufficient 1.3 (1.2-1.4) Pancreas Sufficient 1.5 (1.2-1.8) Breast: postmenopausal Sufficient 1.1 (1.1-1.2)§ Corpus uteri Sufficient 7.1 (6.3-8.1) Ovary Sufficient 1.1 (1.1-1.2) Kidney: renal-cell Sufficient 1.8 (1.7-1.9) Meningioma Sufficient 1.5 (1.3-1.8) Thyroid Sufficient 1.1 (1.0-1.1)§ Multiple myeloma Sufficient 1.5 (1.2-2.0) Male breast cancer Limited NA Fatal prostate cancer Limited NA Diffuse large B-cell lymphoma Limited NA Esophagus: squamous-cell carcinoma Inadequate NA Gastric noncardia Inadequate NA Extrahepatic biliary tract Inadequate NA Lung Inadequate NA Skin: cutaneous melanoma Inadequate NA Testis Inadequate NA Urinary bladder Inadequate NA Brain or spinal cord: glioma Inadequate NA BMI denotes body-mass index, CI confidence interval, and NA not applicable. Sufficient evidence indicates that the International Agency for Research on Cancer Handbook Working Group considers that a preventive relationship has been established between the : case, the absence of excess body fatness) and the risk of cancer in humans - that is, a preventive association has been observed in studies in which chance, bias, and confounding could 1 confidence. Limited evidence indicates that a reduced risk of cancer is associated with the intervention for which a preventive effect is considered credible by the working group, but chai
Nutrizione e cancro 6 di 46U
Obesity and cancer: inflammation bridges the two
Meccanismi di collegamento tra obesità e cancro
Università San Raffaele Roma Massimiliano Caprio HHS Public Access Author manuscript Curr Opin Pharmacol. Author manuscript; available in PMC 2017 August 01. Published in final edited form as: Curr Opin Pharmacol. 2016 August ; 29: 77-89. doi:10.1016/j.coph.2016.07.005. Obesity and cancer: inflammation bridges the two Ryan Kolb1, Fayyaz S. Sutterwala6, and Weizhou Zhang1,2,3,4,5 Obesity leads to macrophage infiltration and inflammation in white adipose tissue in the breast. Inflammatory cytokines promote the upregulation of aromatase and increase production of estrogens in stromal cells of the breast. OBESITY Insulin Resistance 1 Estrogens · | insulin, IGF-1 Inflammation . IL-1B . CCL2 · IL-8 . CCL5 · IL-6 . TNF-a Macrophage Infiltration Adipokine Imbalance · | Leptin · Į Adiponectin Breast cancer tumorigenesis and progression Obesity-associated inflammation is also involved in the development of insulin resistance and increased IGF1, which is a mitogen for breast epithelial cells. Obesity also leads to an increase in leptin and a decrease in adiponectin. Leptin expression is induced by inflammatory cytokines and can induce expression of inflammatory cytokines leading to increased inflammation. All of these factors contribute to a pro-tumorigenic microenvironment
Nutrizione e cancro 7 di 46U
Obesity and Energy Balance Considerations in Triple Negative Breast Cancer
Profilo infiammatorio e progressione del cancro al seno
Università San Raffaele Roma Massimiliano Caprio HHS Public Access Author manuscript Cancer J. Author manuscript; available in PMC 2022 January 01. Published in final edited form as: Cancer J. 2021 ; 27(1): 17-24. doi:10.1097/PPO.0000000000000502. Obesity and Energy Balance Considerations in Triple Negative Breast Cancer Elizabeth R. Berger1,3, Neil M. Iyengar2,4 Anti-Inflammatory Profile IFN-y Lobe Increased Adiponectin Decreased Leptin Increased IL-4, IL-10, IL-13, IFN-y Pro-Inflammatory Profile Increased Leptin Decreased adiponectin Increased TNF-alpha, IL-6, IL-8, IL-12, Ducts "otic ocyte Crown-like Structure M2 Macrophage Dominated (Lean State) M2 Macrophage Dominated (Obese/Inflammatory State) Adipocytes Caloric Excess Adipose Hypertrophy Secretory Dysfunction Hypoxia Oxidative Stress Aggressive Breast Cancer Cells Increased Proliferation Increased Migration Increased Invasion Increased Beta-Oxidation WEIGHT GAIN FIGURE 1. Pathophysiology of the obesity-breast cancer link.
Nutrizione e cancro 8 di 46U
Drilling for Oil: Tumor-Surrounding Adipocytes Fueling Cancer
Ruolo degli adipociti nel cancro alla prostata
Università San Raffaele Roma Massimiliano Caprio Drilling for Oil: Tumor-Surrounding Adipocytes Fueling Cancer Camille Attane . Catherine Muller Published: March 26, 2020 . DOI: https://doi.org/10.1016/j.trecan.2020.03.001 Lipids from Adipocytes Support Prostate Cancer Progression Lean TG Lipolysis o FFA - Lung FFA # Invasive tumor cell ROS MMP14 NOX5 HIF1 200 Spine ROS Lymph node NOX5 FFA Bone FFA Periprostatic adipose tissue Lipolysis) TG Obese Mol Cancer Res; 17(3) March 2019
Nutrizione e cancro 9 di 46 Metastasis Brain Prostate Primary tumor LiverU
Tumor Progression Promoted by Tumor Cell Uptake of Lipid Released by Adipocytes
Meccanismi di progressione tumorale e lipidi
Università San Raffaele Roma Massimiliano Caprio Tumor Progression Promoted by Tumor Cell Uptake of Lipid Released by Adipocytes at the Invasive Front Dedifferentiation Delipidation Activated phenotype LIPOLYSIS cancer-associated adipocytes CAA Adipocyte LIPOLYTIC SIGNALS LIPID RELEASE V Catecholamines V FFA V Proinflammatory cytokines V EV-contained FFA Increased proliferation and survival V Adrenomedullin / Other signals Increased invasion Cancer cell Lipid transfer Metabolic remodeling Resistance to chemotherapy lipid metabolic reprogramming Tumor cells release lipolytic signals to transform adipocytes into cancer-associated adipocytes that exhibit dedifferentiation, delipidation, and an activated phenotype. In turn, adipocytes liberate free fatty acid , but also extracellular vesicle (EV)-contained FFA. Such lipids are internalized by tumor cells and trigger lipid metabolic reprogramming to promote tumor progression.
Nutrizione e cancro 10 di 46 Other lipidsU
Nutrition and Cancer Risk from the Viewpoint of the Intestinal Microbiome
Deterioramento ambientale cellulare e disbiosi
Università San Raffaele Roma Massimiliano Caprio nutrients MDPI Review Nutrition and Cancer Risk from the Viewpoint of the Intestinal Microbiome Yoshimu Tanaka 1,2,*, Shin Shimizu 2,3, Masahiko Shirotani 2,4, Kensho Yorozu 2,5, Kunihiro Kitamura 2,6, Masayuki Oehorumu 2,7, Yuichi Kawai 2,8 and Yoshitaka Fukuzawa 2,9 Dysbiosis (the alteration and simplification of the intestinal microbiota composition) can induce abnormal functioning of the immune system and chronic inflammation, causing carcinogenesis and the promotion of cancer processes. Cellular environmental deterioration Loss of diversity and imbalance of gut microbiota Imbalance of minerals Contact with carcinogenic and toxic substances Overeating, Obesity and increase of saturated fatty acids Lack of exercise and lymphatic perfusion Excessive stress, lack of blood stream and hypofunction of immunity Hypofunction of mitochondria Decrease of use of energy Deficiency of vitamins related to metabolism Cellular Ca excess and Mg deficiency Continuous ischemia and hypoxia Exposure to radiation, ultraviolet, active oxygen and mutagenic substances Bacterial infection Endoplasmic reticulum stress Disorder of protein distribution Increase in abnormal protein Overconsumption of animal protein Excessive saturated fatty acid Deterioration of fluidity of cellular membrane Carcinogenesis Chromosomal abnormalitygene mutation Physical and mental stress Predominant state of sympathetic nervous activation Weakness of immune system Development of cancer
Nutrizione e cancro 11 di 46